Free Anesthesia In-Training Exam Sample Questions
See why TrueLearn is a trusted resource for thousands of medical students and residents. We understand that it’s all about the content. That’s why we have high-yield anesthesia practice questions written and screened by physician authors, which are regularly updated to ensure our SmartBanks stay up-to-date with exam blueprint changes. Below is a free anesthesia exam sample question to showcase what we mean.
Try This ABA ITE Sample Question from the 2026 New Edition
Which of the following is an absolute contraindication to neuraxial anesthesia?
A. Aortic stenosis
B. Increased intracranial pressure due to intracranial mass
C. Inherited coagulopathy
The Answer and Explanation
Did you get it right? The correct answer is B.
Increased intracranial pressure caused by an intracranial mass is an absolute contraindication to neuraxial anesthesia because brainstem herniation can subsequently ensue.
Proper patient selection for neuraxial anesthesia is of the utmost importance. Absolute contraindications to neuraxial anesthesia include increased intracranial pressure (except in cases of idiopathic intracranial pressure), patient refusal, infection at the site of injection, uncorrected hypovolemia, and allergy to any drugs involved. Relative contraindications should be weighed against the potential benefits and include coagulopathy, sepsis, fixed cardiac output states, aortic stenosis, and neurological diseases. Preexisting neurologic conditions may also be considered a relative contraindication to neuraxial anesthesia, but the individual patient’s disease severity needs to be considered.
| Contraindications to Spinal Anesthesia | |
| Absolute Contraindications | Relative Contraindications |
| – Patient refusal – Infection at the site of injection – Uncorrected hypovolemia – Allergy to drugs used – Increased intracranial pressure* | – Coagulopathy – Sepsis – Fixed cardiac output states – Aortic stenosis – Indeterminate neurological disease** |
| * Except in cases of idiopathic intracranial pressure. ** Such as multiple sclerosis and other demyelinating diseases. | |
Incorrect Answer Explanations
Answer A: Aortic stenosis is a relative contraindication to neuraxial anesthesia. Since patients with aortic stenosis are preload dependent, the speed and extent to which systemic vascular resistance can be reduced in spinal anesthesia can lead to a rapid decrease in coronary perfusion. Thus, each case should be assessed individually based on the severity of the disease. An epidural or intrathecal catheter can be considered, and small doses can be titrated over a longer time to avoid drastic hemodynamic changes.
Answer C: Inherited coagulopathy, such as hemophilia, idiopathic thrombocytopenic purpura, or von Willebrand disease, is a relative contraindication to neuraxial anesthesia. There are no minimum safe levels for these factors or platelet counts. However, hemorrhagic complications are infrequent if the levels are > 0.5 international units/mL for factor VIII or von Willebrand factor or when the platelet count is > 50,000/μL.
Bottom Line
Absolute contraindications to neuraxial anesthesia include patient refusal, infection at the injection site, uncorrected hypovolemia, allergy to any drugs involved, or increased intracranial pressure (except in cases of idiopathic intracranial pressure).
Another Free Anesthesia ITE Sample Question
Which of the following MOST accurately describes the mechanism of neuraxial opioid administration?
A. Primarily leads to systemic absorption and subsequent central effects that inhibit nociception
B. Produces locally mediated inhibitory effects on the spinal cord only
C. Reduces ascending nociceptive signaling via binding in the substantia gelatinosa
The Answer and Explanation
Did you get it right? The correct answer is C.
Neuraxial opioid administration results in multiple effects, including the inhibition of nociceptive nerve impulses via ligand-mediated binding within the substantia gelatinosa of the spinal cord, resulting in reduced neurotransmitter release. Direct effects on the medulla and periaqueductal gray areas that project neurons into the spinal cord cause inhibition of ascending pain transmission from the dorsal horn as well.
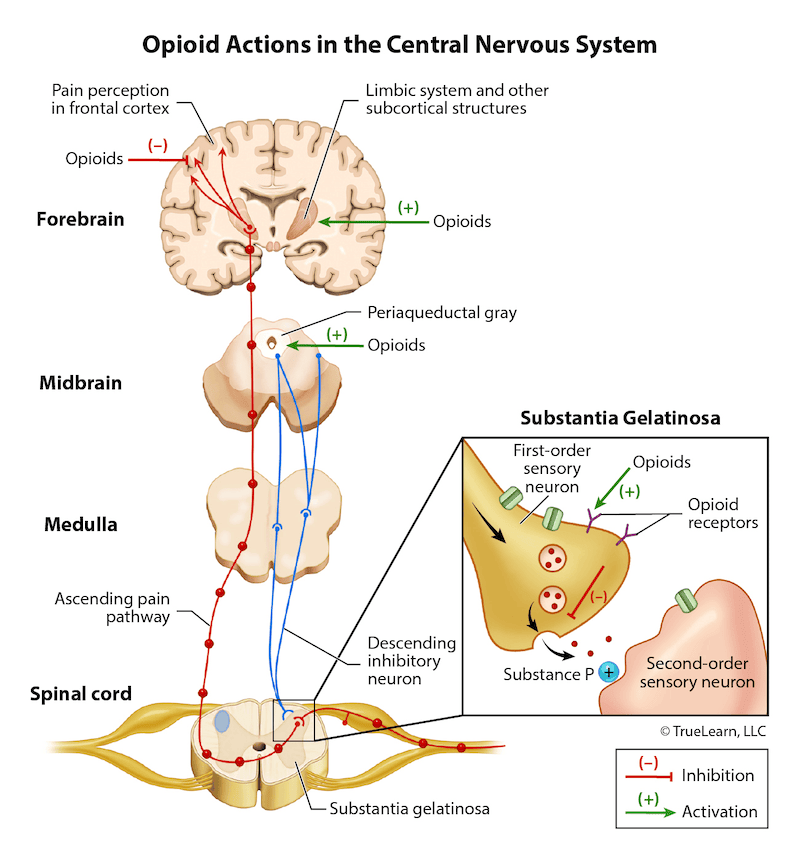
Systemic opioid administration produces a complex interplay between several brain areas that results in analgesia. Primarily, however, neuraxial opioids have a direct effect on the spinal cord, although there is evidence that systemic absorption also occurs and can produce effects in areas of the brain. During neuraxial opioid administration, the binding of neuraxial opioids at presynaptic and postsynaptic neurons within the substantia gelatinosa of the spinal cord lead to suppression of substance P and glutamate secretion. The transmission of nociceptive information arising from the dorsal horn toward the brain (ie, ascending pathway) is inhibited via this process. Correspondingly, descending nociceptive signaling from the midbrain and periaqueductal gray area inhibit the flow of ascending nociceptive firing from dorsal horn neurons through inhibitory projections into the spinal cord. Several brain areas are involved in pain modulation outside the spinal cord. These areas include the cingulate cortex, insula, orbitofrontal cortex, and the brainstem. Positron emission scan results provide evidence that the descending nociceptive signaling ending in the dorsal horn from areas such as the periaqueductal gray and rostral ventromedial medulla are disrupted by the administration of opioids and play a role in nociceptive inhibition as well. Clearly, there is an incredibly complex interplay between human neurophysiology and opioid receptor–binding substances. Neuraxial opioids may produce more pronounced effects in the spinal cord, but systemic effects may also be responsible for some of the analgesic qualities of neuraxial infusion of the drugs.
Incorrect Answer Explanations
Answer A: Although some theorists have suggested the infusion of opioids does lead to systemic absorption, the primary nociceptive inhibition after neuraxial infusion results from local uptake by the spinal cord. In the case of less lipid-soluble opioids, the brainstem and brain will see the effects of these medications via movement through the central spinal fluid to the brain. The extended effects and late respiratory depression caused by morphine demonstrate this behavior of lipid-insoluble opioids. Answer B: Some systemic absorption does occur after neuraxial infusion, and the movement of opioids up the spinal column and to the brainstem and brain via the cerebral spinal fluid also occurs, resulting in analgesic effects as well.
Bottom Line
Neuraxial opioids have a complex mechanism of action, primarily mediated by the inhibition of ascending nociceptive nerve impulses from the spinal cord via ligand-mediated binding within the substantia gelatinosa. The reduction of substance P and glutamate release at presynaptic and postsynaptic neurons within the spinal cord is primarily responsible for reduced pain transmission with neuraxial opioids. Effects in the brain and brainstem also occur through systemic absorption and passage through the cerebrospinal fluid, resulting in projections into the spinal cord that inhibit pain transmission from the dorsal horn as well. For more information, see:
- American Board of Anesthesiology Keyword. “Neuraxial opioids: Mechanism (A)”
- Gropper M, et al. Miller’s Anesthesia. Ch. 45: Spinal, Epidural, and Caudal Anesthesia. Section: Opioids. 9th ed.
- George MJ. The site of action of epidurally administered opioids and its relevance to postoperative pain management. Anaesthesia, 2006;61:659-664.