Free COMLEX Level 2 Practice Questions
We understand that it’s all about the content. That’s why we have high-yield practice questions written and screened by physician authors that are updated on a regular basis to ensure our COMLEX Level 2 CE SmartBank stays up-to-date with exam blueprint changes.
See why TrueLearn is a trusted resource for thousands of medical students and residents.
Here’s Your Free COMLEX Level 2 Practice Question
A 60-year-old male presents to the office with shortness of breath at rest and a productive cough for the past 4 months. He has smoked 1 pack of cigarettes per day for the past 40 years. Physical examination reveals diffuse wheezing and crackles. A chest radiograph is obtained and reveals bilateral lung hyperinflation.
Further diagnostic testing is most likely to reveal which of the following?
A. Elevated hematocrit
B. Elevated white blood cell count
C. Increased FEV1/FVC ratio
D. Left-sided heart failure
E. Respiratory alkalosis
The Answer and Explanation
Did you get it right? The correct answer is A.
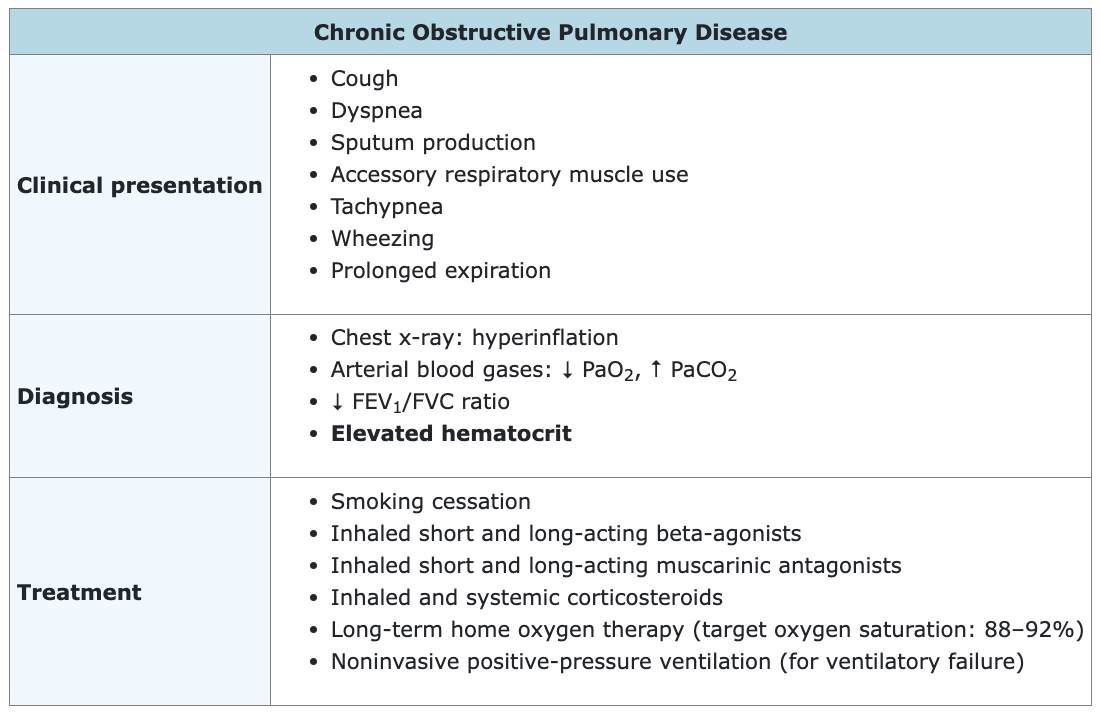
This patient likely has chronic obstructive pulmonary disease (COPD), as suggested by his symptoms (dyspnea, productive cough), wheezing and crackles on examination, hyperinflated lungs on x-ray, and extensive smoking history (a major risk factor for COPD). COPD includes both chronic bronchitis and emphysema. With COPD, airway narrowing results in impaired air flow, especially during exhalation, and leads to premature closure of small airways during exhalation, resulting in air trapping and increased lung volumes.
Dyspnea and a productive cough are the most common symptoms of COPD. In addition to wheezing and crackles, physical examination may also reveal decreased breath sounds, prolonged expiration, accessory respiratory muscle use, and tachypnea. Hyperinflation of the lungs on chest x-ray is common, especially in patients with emphysema.
Arterial blood gases in patients with COPD will usually show at least some degree of hypoxia, and CO2 retention will be observed in severe disease. Pulmonary function testing will show a decreased FEV1/FVC ratio, characteristic of all obstructive lung diseases. Moderate to severe COPD can lead to secondary polycythemia (ie, an elevated hematocrit), which is mostly due to chronic hypoxia. Hypoxia from any cause increases the release of erythropoietin from the kidneys, which in turn stimulates red blood cell production in the bone marrow. Carbon monoxide released from cigarette smoke also increases erythropoietin production, contributing to the polycythemia.
Treatment of COPD includes inhaled bronchodilators, inhaled and systemic corticosteroids, and respiratory support if necessary (eg, supplemental oxygen, noninvasive positive-pressure ventilation). As smoking is the main risk factor for COPD, smoking cessation is recommended for all patients with COPD. Smoking cessation has been demonstrated to slow disease progression and decrease mortality. Other measures shown to reduce mortality include long-term oxygen therapy and lung reduction surgery (when indicated).
The below image shows a chest radiograph of a patient with COPD (specifically, emphysema). Note the bilateral lung hyperinflation and accompanying narrow cardiac silhouette.

Incorrect Answer Explanations
Answer B: An elevated white blood cell count would be seen if the patient had an acute infection. Although pneumonia can present with dyspnea and a productive cough, this patient has no other evidence of infection in general (eg, fever) or pneumonia specifically (eg, pulmonary infiltrates on chest x-ray).
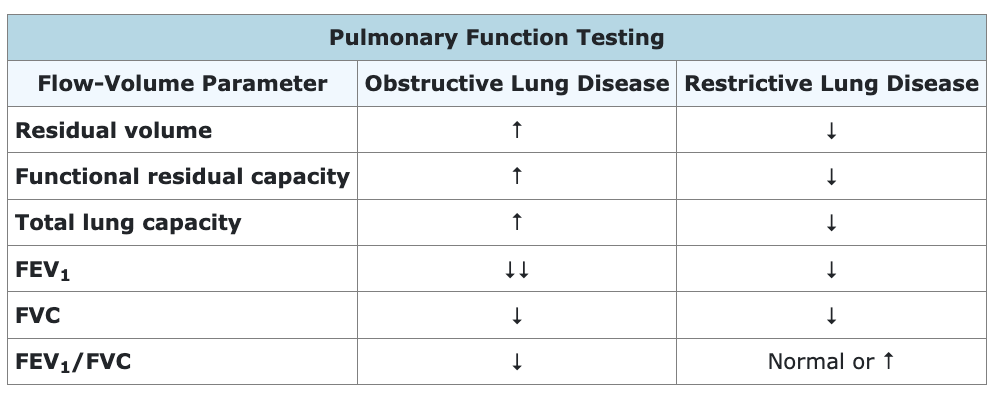
Answer C: An increased (or normal) FEV1/FVC ratio would be seen with restrictive lung diseases, such as idiopathic pulmonary fibrosis or pneumoconiosis. Both FVC and FEV1 are decreased in restrictive lung diseases (along with decreased lung volumes), but the speed of air flow during exhalation is generally maintained because of the high elastic recoil of the lungs. Thus, the decrease in FEV1 is the same or less than the reduction in FVC, resulting in a normal or increased FEV1/FVC ratio. FVC and FEV1 are also both decreased in COPD, but airway obstruction significantly reduces the speed of air flow during exhalation, causing a greater reduction in FEV1 than in FVC and resulting in a decreased FEV1/FVC ratio.
Answer D: Left-sided heart failure is most commonly seen in patients with systemic arterial hypertension or coronary artery disease. Right-sided heart failure is a more likely finding in patients with COPD, as chronic hypoxia leads to chronic hypoxic pulmonary vasoconstriction, resulting in pulmonary arterial hypertension.
Answer E: Respiratory alkalosis occurs with conditions causing hyperventilation, such as panic attacks, high altitude, early salicylate poisoning, and pulmonary embolism. By contrast, COPD is characterized by respiratory acidosis because of increased dead space ventilation (ie, areas of increased V/Q), leading to CO2 retention. Compensatory metabolic alkalosis is also common, as the kidneys retain bicarbonate in an attempt to return the pH to normal.
Bottom Line: Chronic obstructive pulmonary disease can lead to hypoxia, which increases the release of erythropoietin from the kidneys. This in turn causes secondary polycythemia, with an elevated hematocrit.
COMBANK Insight: Pulmonary diseases can be divided into 2 broad groups: obstructive lung disease and restrictive lung disease. Pulmonary function testing is a useful way to differentiate these groups.
For more information, see:
Chronic obstructive pulmonary disease: definition, clinical manifestations, diagnosis, and staging: UpToDate
Chronic obstructive pulmonary disease: StatPearls
Image sources:
Chest x-ray in COPD: Wikimedia Commons
![[On-Demand Webinar] COMLEX Level 2 PE Overview](https://truelearn.com/wp-content/uploads/2020/11/Featured-Image_Webinar.png)
