Free COMLEX Level 2 Practice Questions
We understand that it’s all about the content. That’s why we have high-yield practice questions written and screened by physician authors that are updated on a regular basis to ensure our COMLEX Level 2 CE SmartBank stays up-to-date with exam blueprint changes.
See why TrueLearn is a trusted resource for thousands of medical students and residents.
Here’s Your Free COMLEX Level 2 Practice Question
A 58-year-old man presents to the emergency department with a 2-day history of blurry vision and light-headedness. Upon waking today, his vision was significantly worse, causing him difficulty driving to work. His history reveals poorly controlled diabetes and hypertension due to medication non-adherence. He is prescribed metformin, lisinopril, clonidine, and amlodipine. He has not seen his physician in over 6 months. Vital signs reveal:
| Blood pressure | 195/120 mmHg |
| Heart rate | 88/min |
| Respiratory rate | 16/min |
| Oxygen saturation | 99% on room air |
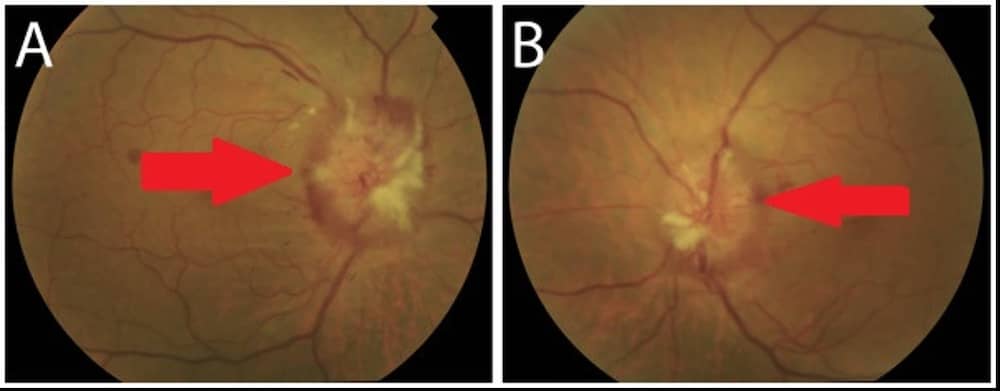
Physical examination reveals his pupils are equal and reactive to light bilaterally, extraocular movements are intact, and conjunctiva are normal. He can differentiate colors and shapes but can only read only the top line of a visual acuity chart with both eyes. An image of his fundoscopic examination is shown in the exhibit. The most likely cause of this patient’s presentation is
- A. central retinal artery occlusion
- B. central retinal vein occlusion
- C. hyperglycemia
- D. hypertensive emergency
- E. occipital lobe stroke
The Answer and Explanation
The correct answer is: D
This patient is presenting with hypertensive emergency, defined as systolic blood pressure ≥ 180 mmHg and/or diastolic blood pressure ≥ 120 mmHg with signs of end-organ damage. This patient has likely not been taking his blood pressure medication, causing significantly elevated blood pressure. He may also have developed rebound hypertension from his intermittent dosing of clonidine. This patient’s end-organ damage includes papilledema, which is swelling of the optic discs due to increased intracranial pressures, which is seen on fundoscopy.
The presence of end-organ damage is what differentiates hypertensive emergency from severe asymptomatic hypertension. Examples of end-organ damage include cardiovascular, renal, or central nervous system effects. Hypertensive emergency causes damage by characteristic fibrinoid necrosis of arterioles. It also causes the dilatation of cerebral arteries (another pathological process that takes place after the normal autoregulation is unable to maintain a normal blood pressure of cerebral blood flow is disturbed).
Causes of hypertensive emergency include:
- Pregnancy: severe preeclampsia
- Sympathetic drugs: cocaine and amphetamines
- Withdrawal: alcohol, short-acting beta-blockers (eg, propranolol), barbiturates, benzodiazepines
- Psychiatric medicines: serotonin syndrome, neuroleptic malignant syndrome, hypertensive crisis (monoamine oxidase inhibitors)
- Catecholamine excess: pheochromocytoma
- Noncompliance: rebound hypertension from stopping medications (eg, clonidine)
Although the patient’s blood pressure must be lowered to prevent further end-organ damage, it must not be lowered too abruptly. Rapid reduction can increase the risk of relative cerebral ischemia, which results from hypoperfusion as the cerebral arteries need time to autoregulate.
For most hypertensive emergencies, mean arterial pressure should be reduced gradually by about 10–20% in the first hour and a further 5–15% over the next 23 hours. Exceptions to this include intracranial hemorrhage and aortic dissection, which require a much more aggressive rate of pressure reduction due to the high mortality risk.
End-Organ Damage Commonly Associated With Hypertensive Emergency
| System | Findings |
| Neurologic | Agitation, delirium, stupor, seizures, encephalopathyIncreased intracranial pressure (intractable nausea/vomiting)Intracranial hemorrhage |
| Ophthalmologic | Fresh flame hemorrhages, exudates (cotton-wool spots), or papilledema |
| Cardiac | Elevated troponins and chest pain from demand cardiac ischemiaAortic dissection |
| Respiratory | Dyspnea related to pulmonary edema |
| Renal | Acute hypertensive nephrosclerosisAcute kidney injury |
The below images demonstrate bilateral papilledema in the optic disc (red arrows). This is due to increased intracranial pressure as a result of a hypertensive emergency.
Incorrect Answer Explanations
Answer A: A central retinal artery occlusion (CRAO) is a rare disorder characterized by acute painless monocular vision loss. Retinal ischemia may be seen on fundoscopy (cherry-red fovea). This condition is considered a type of stroke and is managed similarly. There are many etiologies, including atherosclerosis, embolism, and vascular disease. Embolic causes include atrial fibrillation, infective endocarditis, and paradoxical deep vein thrombosis. CRAO leads to sudden symptoms, often with other focal neurologic deficits. This patient’s binocular vision changes, papilledema, and blood pressure ≥ 180/120 mmHg are more characteristic of hypertensive emergency than an embolic phenomenon.
Answer B: A central retinal vein occlusion (CRVO) occurs due to thrombus formation within the central retinal vein at the level of the lamina cribrosa of the optic nerve, leading to the involvement of the entire retina. Patients are rarely asymptomatic and usually present with acute onset of painless blurred vision in one eye. Clinically, the pupillary examination can be normal but typically demonstrates an ipsilateral relative afferent pupillary defect in cases of nonperfused CRVO. The fundus examination has the classic appearance of “blood and thunder” and usually will reveal retinal hemorrhages, edema, dilated retinal veins, and possibly cotton-wool spots. This constellation of findings was not present in this patient, making CRVO unlikely.
Answer C: Hyperglycemia, both acute and chronic, can cause blurriness and vision changes, but it will not cause the ocular findings of papilledema noted in this patient.
Answer E: An occipital lobe stroke can occur from occlusions usually in the vertebrobasilar system and can present with vision changes. These vision changes are usually visual field deficits (hemianopia) along with accompanied oculomotor and pupillary abnormalities. This patient does not have vision loss in one eye nor does he have hemianopia. In addition, papilledema is not commonly seen in occipital strokes.
Bottom Line: Hypertensive emergency is defined as systolic blood pressure ≥ 180 mmHg and/or diastolic blood pressure ≥ 120 mmHg with end-organ damage. Papilledema may be seen, which is swelling of the optic discs due to increased intracranial pressures.
For more information, see:
- Drugs used for the treatment of hypertensive emergencies: UpToDate
- Evaluation and treatment of hypertensive emergencies in adults: UpToDate
- Image sources: Bilateral papilledema (modified in explanation): BMC Ophthalmol
![[On-Demand Webinar] COMLEX Level 2 PE Overview](https://truelearn.com/wp-content/uploads/2020/11/Featured-Image_Webinar.png)
