Free Sample FNP Practice Questions
See why TrueLearn is a trusted resource for thousands of medical students and residents. We understand that it’s all about the content. That’s why we have high-yield family nurse practitioner practice questions written and screened by high-performing physician authors, which are updated on a regular basis to ensure our SmartBanks stay up-to-date with exam blueprint changes. Below is a free FNP sample question so you can see what we mean.
Your First Free FNP Practice Question
A 50-year-old female is rushed to the emergency department after she was found unresponsive as a result of being an unrestrained driver in a motor vehicle accident that occurred on the highway. Other drivers that witnessed the accident state that she may have gone through her windshield. The patient’s vitals are stable and her Glasgow Coma Scale score is remarkably now 12. Her CT head and neck without contrast are unremarkable for evidence of hematoma or skull fracture. She becomes increasingly more alert after close observation, and she complains of a significant headache and she feels very drowsy. After providing the patient with appropriate analgesia, the osteopathic nurse practitioner decided to evaluate her for possible osteopathic treatment. He has difficulty establishing the flexion and extension phases of the cranium, but the patient’s cranial rhythmic impulse is 2 (normal 10-14).
What is the patient’s most likely osteopathic diagnosis?
- A. Inferior vertical strain
- B. Left lateral strain
- C. Left sidebending rotation
- D. Sphenobasilar synchondrosis compression
- E. Superior vertical strain
The Answer and Explanation
The correct answer is: D
A sphenobasilar synchondrosis (SBS) compression is a non-physiological strain pattern of the cranium. The sphenoidal base and base of the occiput are compressed together as a result of trauma. Various examples of SBS trauma include malpresentation during birth, such as a baby that presents face-first during labor or a high-velocity car accident with injury to the head. An indirect traumatic insult could result from injury to the sacrum due to the primary respiratory mechanism described above. The amount of flexion and extension of the sphenoid and occiput is minimal to undetectable, which is appreciated as a decreased CRI. A CV4 technique, which involves gentle compressive force in the area of the fourth ventricle to help increase CRI amplitude, balance autonomic nervous system dysfunction, and increase overall motion.
The primary respiratory mechanism (PRM) is a term used to describe the motion that occurs between the cranium, spinal cord, and sacrum as an entire unit of function and motility. The PRM is composed of the spinal cord, cerebrospinal fluid, dural membranes, cranial bones, and the sacrum. Each component offers a contribution to the overall respiratory mechanism, such as the inherent motility of the brain and spinal cord with cerebrospinal fluid fluctuations and movement of the intracranial and intraspinal membranes. These components also fluctuate under the influence of the movement of the cranial bones and sacrum. This concert of movement can be appreciated in the form of a cranial rhythmic impulse (CRI), which is a palpable pulsation appreciated by the cranial vault hold.
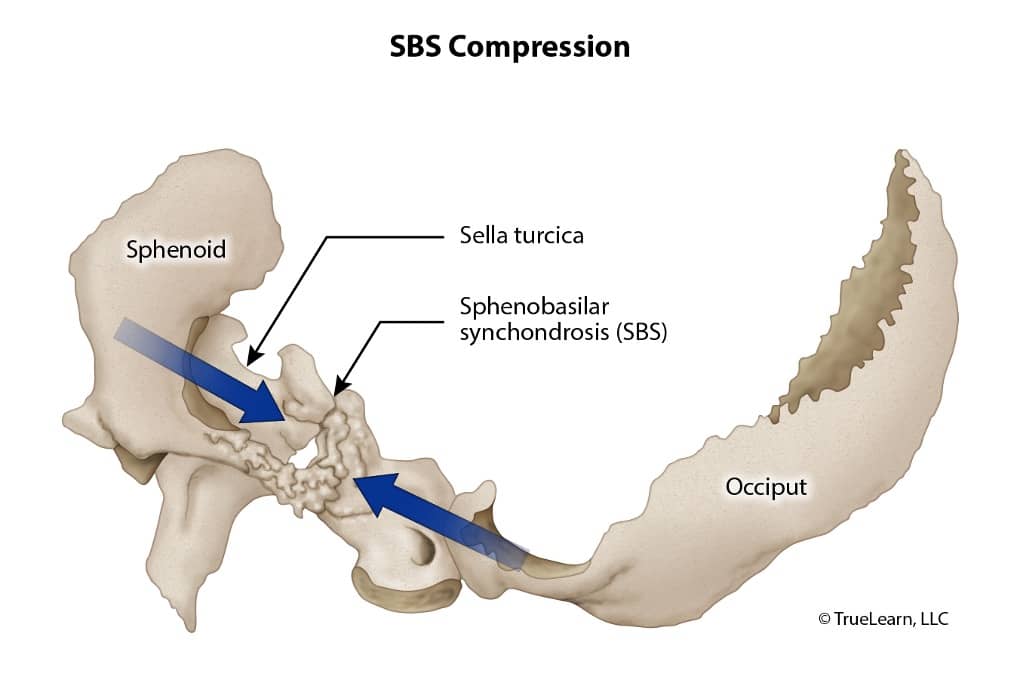
The cranial vault hold involves placing the index finger on the greater wing of the sphenoid, the middle finger on the temporal bone (in front of the ear), the ring finger on the mastoid, and the pinky finger on the flat surface of the occiput. This particular finger placement allows the nurse practitioner to appreciate this motility and detect any abnormality in the normal, physiologic expansion and contraction of the cranium. Normally, the midline bones, such as the sphenoid and occiput, move through a flexion phase while paired bones (i.e. temporal bones) exhibit external rotation. Conversely, during the extension phase, the midline bones move into extension while the paired bones exhibit internal rotation. A variety of possible strains of the cranial bones include torsion, side-bending rotation, vertical strain, lateral strain, and compression. These strains are created by asynchronous and asymmetric movement about the junction between the sphenoid and occiput.
Incorrect Answer Explanations
Answer A: An inferior vertical strain is a non-physiological strain pattern that is a result of a direct force that causes displacement of the base of the sphenoid and the base of the occiput. It causes rotation of the sphenoid and occiput in the same direction about two transverse axes. It is named for the position of the sphenoid base in relation to the base of the occiput, which in this case would be inferiorly displaced.
Answer B: A lateral strain, unlike torsions and side-bending rotation strains, is non-physiologic and is the result of direct impact to the sphenobasilar synchondroses (SBS). The sphenoid and occiput end up rotating in the same direction along two vertical axes. The direction of the strain is named for the direction of the sphenoidal base in relation to the base of the occiput. The opposite index and pinky fingers move in the same direction. For example, if the index fingers are both shifted right and the pink fingers are shifted left, then the base of the sphenoid has shifted to the left and the base of the occiput has shifted right.
Answer C: A left side-bending rotation involves movement along three axes – an anteroposterior axis and two parallel, vertical axes (one through the foramen magnum and one through the center of the sphenoid). The sphenoid and occiput rotate in the same direction on the anteroposterior axis and opposite directions along the two vertical axes. The rotation along the anteroposterior axis creates the rotation component, and the opposite direction of rotation of the sphenoid and occiput along the vertical axes creates the side-bending. A side-bending rotation dysfunction is named for the side of convexity that is formed from the combination of these movements. The nurse practitioner would have appreciated a separation of the left index and pinky during the flexion phase of the SBS (creating a convexity) while the right index finger and pinky would approximate (creating a concavity).
Answer E: A superior vertical strain is a non-physiological strain pattern that is a result of a direct force that causes displacement of the base of the sphenoid and the base of the occiput. It causes rotation of the sphenoid and occiput in the same direction about two transverse axes. It is named for the position of the sphenoid base in relation to the base of the occiput, which in this case would be superiorly displaced. This can occur from any form of trauma to the back of the head, such as falls or blunt force trauma. While using the vault hold, the nurse practitioner’s index fingers move forward and lateral while the pinky fingers move backward and inferior.
Bottom Line
A sphenobasilar synchondrosis (SBS) compression is a non-physiological strain pattern of the cranium. The sphenoidal base and base of the occiput are compressed together as a result of trauma. The amount of flexion and extension of the sphenoid and occiput is minimal to undetectable, which is appreciated as a decreased CRI. The CV4 technique can help relieve the compression and increase motility and CRI.
For more information, see:
- King HH. Osteopathy in the cranial field. Chila A, ed. Foundations of Osteopathic Medicine. 3rd ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2011. pp. 728–748.
- Savarese RG, Capobianco JD, Cox JJ. OMT review: A comprehensive review in osteopathic medicine. 2003.
- Ward RC. Foundation of Osteopathic Medicine. 2nd ed. Philadelphia: Lippincott Williams and Wilkins. 2002.
Get More Free FNP Questions
Ready for another free practice question? Check out the free TrueLearn SmartBank trial. Then whenever you’re ready, take a look at our subscriptions.