3 Free General Surgery Board Review Practice Questions
With the vast amount of knowledge that is potentially testable on the ABS Qualifying Exam (QE), it can be hard to see the forest through the trees. It’s important to take your time when studying. Don’t rush yourself. And get all the help you can by exploring the resources available to you. Below are 3 free general surgery practice questions from TrueLearn’s ABS Qualifying SmartBank to show you want you would get with a subscription.
First Free Board Review Practice Question
A 50-year-old man presents to the surgery clinic with intermittent burning substernal chest pain, particularly when he eats spicy foods. He has been taking omeprazole 20 mg once a day for several months now and reports good relief when he is compliant with his medication, which he admits is difficult for him. Upper endoscopy is performed, which shows a salmon-colored patch of mucosa in the distal esophagus. A biopsy is performed that shows the presence of goblet cells without the presence of dysplasia. Which of the following is the next step in the management of this patient?
- A. increase his omeprazole to 20 mg twice daily
- B. change his medication to famotidine 20 mg daily
- C. repeat EGD in 6 months
- D. refer for endoscopic ablative therapy
- E. workup for antireflux surgery
The Answer and Explanation
The correct answer is: E
In general, acid suppression therapy (ie, proton pump inhibitor [PPI] or histamine blocker [H2 blocker]) is the mainstay of GERD treatment for the first 8 weeks. In Barrett esophagus without dysplasia, once daily dosing with a PPI is recommended as first-line treatment. Twice-daily PPI dosing is generally discouraged unless the patient has Barrett with high-grade dysplasia, esophagitis, or severe persistent GERD symptoms.
SAGES guidelines recommend surgical therapy for GERD in patients with complications such as Barrett esophagus, esophagitis, peptic stricture, and other extraesophageal manifestations (ie, chronic cough, chest pain, aspiration, etc.) associated with GERD that affect the patient’s quality of life. Note that fundoplication alone may or may not reverse Barrett esophagus if already present, but it will at least prevent it from progressing. Appropriate surveillance protocols for Barrett esophagus should be employed as usual. Barrett-associated dysplasia or carcinoma should have the lesion eradicated histologically by endoscopic therapy (ablation for low-grade dysplasia or a combination of ablation and endoscopic mucosal resection for high-grade dysplasia or T1a esophageal adenocarcinoma without lymphovascular invasion) before consideration of antireflux surgery.
For this patient, who has been on a PPI for several months but still has Barrett esophagus, and who is not entirely compliant with his PPI regimen, the next step in the management of this patient is initiate workup for antireflux surgery, which involves assessing for the presence of dysmotility, gastroparesis, hiatal or paraesophageal hernia, and fitness for surgery.
Other common indications for antireflux surgery include:
- Failed medical management (the most frequent indication for antireflux surgery)
- Intolerance or noncompliance with medical management
- Complications of GERD: severe esophagitis and benign peptic stricture
- High-volume reflux: typical GI symptoms (eg, regurgitation); atypical, non-GI symptoms (eg, cough or asthma due to aspiration, dental erosions)
- Chronic cough, chest pain, aspiration, and other extraesophageal manifestations associated with GERD
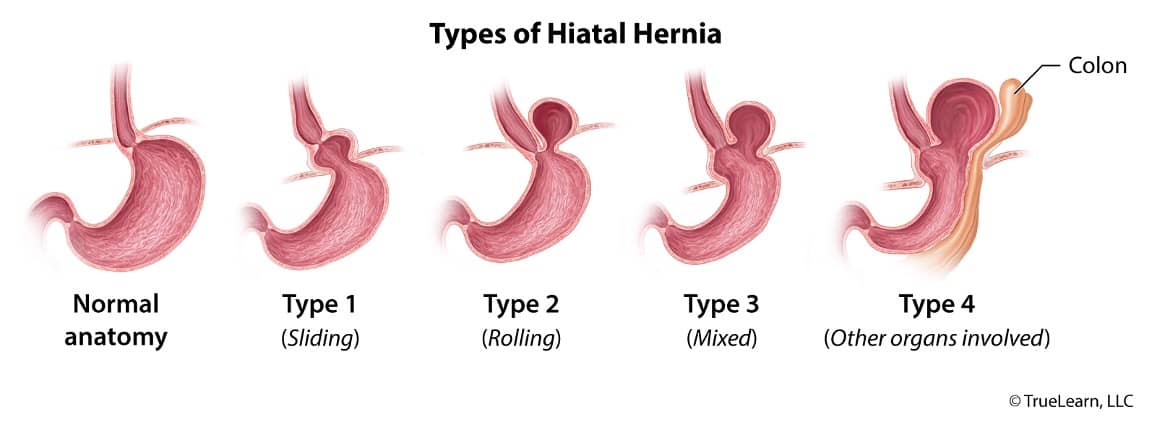
Types of hiatal (or paraesophageal) hernias. Type 1 (sliding hernia): the gastroesophageal junction is “sliding” into the chest. Type 2 (para-esophageal): the gastroesophageal junction remains in the normal anatomic position; however, part of the stomach herniates along the esophagus (para-esophageal). Type 3 (mixed) combines the features of type 1 and type 2: sliding gastroesophageal junction with stomach herniation along the esophagus. Type 4 = type 3 plus other intra-abdominal organs are herniating along the esophagus.
Answer A: Increasing the patient’s omeprazole to twice daily is not generally recommended unless he has severe refractory reflux symptoms, esophagitis, or high-grade dysplasia, none of which apply to him because he reports good relief when he takes his medication, and his EGD showed Barrett without any other concerning features. Additionally, if he is not compliant with once-daily dosing, he is unlikely to be compliant with twice-daily dosing.
Answer B: PPIs are generally the first-line medical therapy in Barrett esophagus. H2 blockers are typically used for milder reflux symptoms without complications of GERD.
Answer C: Endoscopic surveillance should be undertaken in those with Barrett esophagus with concomitant 4-quadrant biopsies. In those with Barrett esophagus without any dysplasia, EGDs should be performed every 3–5 years. In those with Barrett esophagus with low-grade dysplasia, EGDs should be performed every 6 months. In those with Barrett esophagus with high-grade dysplasia, EGDs should be performed every 3 months.
Answer D: Endoscopic ablative therapy (including photodynamic therapy or radiofrequency ablation) should be offered to those with Barrett esophagus with either low- or high-grade dysplasia. Endoscopic mucosal resection should be offered to those with Barrett esophagus with high-grade dysplasia or T1a esophageal adenocarcinoma without lymphovascular invasion.
Bottom Line: Antireflux therapy is recommended for GERD in patients who are noncompliant or have failed medical therapy; or with complications such as Barrett esophagus, esophagitis, peptic stricture, and other extraesophageal manifestations (ie, chronic cough, chest pain, aspiration, etc.) associated with GERD that affect the patient’s quality of life.
For more information, see:
- Chapter 42: Esophageal anatomy and physiology and gastroesophogeal reflux disease. In: Mulholland & Greenfield’s Surgery: Scientific Principles & Practice. 7th ed. Wolters Kluwer; 2021.
- Management of Barrett’s esophagus. In: Cameron AM, Cameron JL, eds. Current Surgical Therapy. 13th ed. Elsevier; 2020:19-25.
- Park JM, Chi KC. Antireflux surgery is equally beneficial in nonerosive and erosive gastroesophageal reflux disease. Ann Surg Treat Res. 2018;95(2):94-99.
- Amadi C, Gatenby P. Barrett’s oesophagus: current controversies. World J Gastroenterol. 2017;23(28):5051-5067.
- SAGES guidelines for the management of hiatal hernias: SAGES
Second Free General Surgery Practice Question
A 35-year-old woman presents with an incidental finding on a trauma CT scan of multiple cystic structures within the pancreas (see below). She is referred for the evaluation of this finding. She is a nonsmoker and a social drinker. She denies any recent weight loss or prior bouts of pancreatitis. Each cyst does not appear to have direct communication with the main pancreatic duct. Percutaneous aspiration of the cystic structure is performed. Analysis of the fluid shows a low level of amylase and a CEA level of 0.35 ng/mL.
What is the most likely diagnosis of this cystic mass?
- A) serous cystadenoma
- B) mucinous cystic neoplasm
- C) pancreatic pseudocyst
- D) pancreatic metastasis
- E) pancreatic adenocarcinoma
The Answer and Explanation
The correct answer is: A
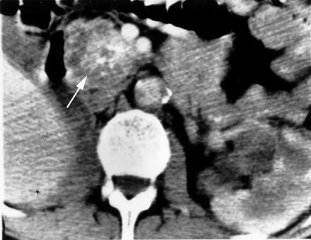
The lack of communication with the main pancreatic duct is classic for both mucinous cystic neoplasms (MCN) and serous cystadenomas (SCN). The central calcification surrounded by multiple cysts (indicated by the arrow in the referenced CT scan) is pathognomonic for SCN and the fluid in the cyst of a SCN is low in CEA, while that in the MCN is high in CEA.
Analysis of Pancreatic Cystic Fluid
| Pseudocyst | Serous Cystadenoma | Mucinous Cystic Neoplasm | Intraductal Papillary Mucinous Neoplasm | |
| Location | Evenly | Evenly | Tail | Head |
| Cytology | Pigmented histocytes | Bland periodic-acid Schiff + | Mucinous | Mucinous |
| Viscosity | Low | Low | Increased | High |
| Amylase | High | Low | Low | High |
| CEA | < 200 ng/mL (typically much less) | < 0.5 ng/mL | > 200 ng/mL | > 200 ng/mL |
| KRAS Mutations | Negative | Negative | Positive | Positive |
Serous cystadenoma of the pancreatic head. This patient demonstrates a typical appearance of a serous cystadenoma (arrow) with central calcifications and innumerable cysts creating a “mass.”
- Answer B: The level of CEA is high in MCNs.
- Answer C: There is no history of alcohol abuse or multiple bouts of pancreatitis that would explain the presence of a pseudocyst. Additionally, the low amylase makes this diagnosis unlikely.
- Answer D: There is no reason to suspect any occult malignancy. Therefore, metastases to the pancreas are unlikely. Also, a metastasis would be solid, not cystic in nature.
- Answer E: Pancreatic adenocarcinoma would not appear cystic on imaging.
Bottom Line: Central calcification surrounded by multiple cysts is pathognomonic for serous cystadenoma. The fluid in the cyst of a serous cystadenoma is low in CEA, while that in a mucinous cystic neoplasm is high in CEA.
TrueLearn Insight: The ability to differentiate pancreatic cystic structures via fluid analysis is important for surgical board exams.
For more information, see:
- Dudeja V, Christein JD, Jensen EH, Vickers SM. Chapter 55: Exocrine pancreas. In: Townsend CM, Beauchamp RD, Evers BM, Mattox K, eds. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 20th ed. Philadelphia, PA: Elsevier; 2017:1520-1525.
- Brugge WR. The use of EUS to diagnose cystic neoplasms of the pancreas. Gastrointest Endosc. 2009;69(2 suppl):S203-S209.
- Image source: Wikimedia Commons
Third Free Practice Question
A 36-year-old male chef is brought to the trauma bay after accidentally stabbing himself at work with a paring knife. He has a 2-cm stab wound to the right of his umbilicus. He is hemodynamically stable. His examination is significant for localized tenderness around the wound without signs of peritonitis. Local wound exploration demonstrates possible violation of the anterior abdominal fascia, but it is not clear if the patient’s peritoneal cavity has been violated due to his body habitus. Which of the following is the best course of action?
- A) discharge from trauma bay
- B) admission for serial abdominal exams
- C) diagnostic peritoneal lavage
- D) CT scan of abdomen and pelvis
- E) exploratory laparotomy
The Answer and Explanation
The correct answer is: B
The question presents a scenario of an anterior abdominal stab wound. The anterior abdomen is the area from the costal margins to the inguinal ligaments between the anterior axillary lines (see image).
Abdominal anatomy with the anterior abdomen bounded by asterisks.
Data have shown that anterior stab wounds only violate the peritoneal cavity a minority of the time (approximately 25-33%). Even in patients with peritoneal penetration, only 50% will present with indications for a laparotomy. In the remaining 50%, only half will become symptomatic and require a laparotomy. Thus, a push has been made in the past few decades for selective nonoperative management of anterior abdominal stab wounds to avoid the morbidity of non-therapeutic laparotomy.
A local wound exploration under semi-sterile conditions is the first step. If it can be confirmed that violation of the anterior abdominal fascia has not occurred, the wound is irrigated, a tetanus immunization is administered, and the patient is discharged. In most centers, a hemodynamically stable patient without peritonitis with penetration of the anterior aponeurosis or peritoneum will undergo serial physical examinations for 24 hours. Almost all patients with continued intraperitoneal bleeding or peritonitis from hollow viscus injury will become symptomatic within 6 to 16 hours, which should then prompt laparotomy.
The incidence of obesity is increasing in the population and therefore is encountered more often in the trauma population. At times, abdominal examinations may be difficult in obese patients. However, the physician is still able to detect the presence or absence of peritoneal signs either by palpation or percussion. On the other hand, local wound exploration is usually done in the trauma bay of the ER with less than ideal lighting and usually uses a small incision in which the surgeon is trying to navigate through several centimeters of adipose tissue in an obese patient to see the fascia and therefore may not see any violation clearly.
A study by Bloom et al. in 2015 concluded that admission and serial abdominal examinations (looking for signs of peritonitis or worsening of findings) in obese trauma patients who were the victims of penetrating abdominal traumas is a preferred approach to immediate exploratory laparotomy, which is preferred in thinner trauma patients who had suffered penetrating abdominal trauma.
- Answer A: Discharge from the trauma bay without observation would be inappropriate in this patient. If the patient’s anterior abdominal fascia were confirmed to be intact, discharge from the trauma bay would be acceptable.
- Answer C: Diagnostic peritoneal lavage (DPL) involves lavaging the peritoneal cavity with warm saline through a small incision made around the umbilicus to determine if there are any intra-abdominal injuries. Enthusiasm for DPL has waned over time due to inexperience in many centers and the possibility of false-positive results from intraperitoneal blood related to injury to the anterior abdominal wall. The focused assessment with sonography for trauma (FAST) exam has largely replaced the use of DPL in most centers.
- Answer D: CT scan is utilized in cases where the patient is not alert and able to undergo a reliable abdominal examination. In many cases, it can show a fascial defect but not in all cases (depending on body habitus and CT scan resolution). This patient is able to undergo serial abdominal examinations to show any degree of peritonitis.
- Answer E: In the past few decades, selective nonoperative management of anterior stab wounds in hemodynamically stable patients without signs of peritonitis has become standard of care to avoid the morbidity of non-therapeutic laparotomy. Exploratory laparotomy is reserved for anterior stab wound patients who are hemodynamically unstable or have signs of peritonitis.
Bottom Line: Selective nonoperative management of anterior stab wounds in hemodynamically stable patients without signs of peritonitis has become standard of care to avoid the morbidity of non-therapeutic laparotomy. If the anterior abdominal fascia has been violated on local wound exploration, admission for serial abdominal examinations is the preferred course of action.
For more information, see:
- Feliciano DV. Penetrating abdominal trauma. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. 13th ed. Philadelphia, PA: Elsevier; 2020:1162-1166.
- Martin MJ et al. Evaluation and management of abdominal stab wounds: A Western Trauma Association decisions algorithm. J Trauma Acute Care Surg. 2018; 85(5):1007-1015.
- Bloom MB, Ley EJ, Liou DZ, et al. Impact of body mass index on injury in abdominal stab wounds: implications for management. J Surg Res. 2015;197(1):162-166.
- Image source: Wikimedia Commons
Start Studying with TrueLearn’s ABS Qualifying SmartBank
For hundreds of other general surgery practice questions, along with authoritative answer explanations, illustrative figures and tables, supporting references, focused Bottom Line statements, and test-taking tips, check out our ABS Qualifying question bank.
To learn more about the exam itself, check out our article on everything you need to know for the ABS Qualifying exam.