Free USMLE Step 1 Sample Questions
The following three USMLE Step 1 sample questions from TrueLearn’s SmartBank test some of the high-yield material you’re sure to see on exam day. Each question is followed by an authoritative answer explanation, complete with rich visuals, a focused Bottom Line statement, and supporting references (including page numbers from First Aid for the USMLE Step 1). Finally, each question also includes a unique TrueLearn Insight.
TrueLearn Insights are where our expert author team provides Step-wise strategies and tables to help you master the exam. Inspired by our authors’ own experience studying and tutoring for Step 1, they address common student struggles through detailed insider advice. As a supplement to our thorough answer explanations, TrueLearn Insights provide added value not available from any other USMLE question bank.
For thousands of other high-yield practice questions, along with exam-focused answer explanations, summary tables, figures, Bottom Line statements, and references—plus more exclusive TrueLearn Insights—order a free trial today.
First Step 1 Sample Question: Microbiology
A 5-year-old boy is brought to the emergency department by his mother because of fever and dark urine. His mother states that he was in his usual state of health until 7 days ago, when he had a gastrointestinal illness with bloody diarrhea and vomiting that lasted 2 days. During that time, the mother reports that he was able to continue drinking fluids. Since resolution of the diarrhea, he has appeared tired and sleepy. She notes that he has used the bathroom much less frequently than usual. On examination, the boy is somewhat irritable. His temperature is 38.6°C (101.5°F), pulse is 100/min, respirations are 18/min, and blood pressure is 102/68 mm Hg. Scleral icterus is noted on physical examination. His abdomen is soft and nontender. Laboratory studies show:
| Hemoglobin | 9.2 g/dL |
| Hematocrit | 30% |
| Leukocyte count | 9700/mm3 |
| Platelet count | 60,000/mm3 |
| Prothrombin time | 12 sec |
| Partial thromboplastin time (activated) | 35 sec |
| Serum | |
| Urea nitrogen | 33 mg/dL |
| Creatinine | 1.9 mg/dL |
| Urine | |
| Protein | 1+ |
| Blood | 2+ |
Which of the following is the most likely cause of this patient’s current condition?
- A. Campylobacter jejuni
- B. Escherichia coli O157:H7
- C. Henoch-Schonlein purpura
- D. Shigella flexneri
- E. Staphylococcus aureus enterotoxin
- F. Streptococcus pyogenes
- G. Viral gastroenteritis
Answer & Explanation
The correct answer is: B
| Hemolytic Uremic Syndrome | |
| Pathogenesis | Associated with infection with enterohemorrhagic Escherichia coli and Shigella dysenteriae Results from production of shiga-like toxin and shiga toxin (respectively) Often seen in children |
| Clinical Features | Recent history of bloody diarrhea Triad: 1. Microangiopathic hemolytic anemia → fatigue, jaundice, dark urine 2. Thrombocytopenia → bleeding, bruising, epistaxis 3. Renal dysfunction |
| Laboratory Findings | Hemolytic anemia: 1. Normocytic anemia 2. ↑ Reticulocytes 3. ↑ Lactate dehydrogenase 4. ↑ Total bilirubin 5. ↓ Haptoglobin ↓ Platelets ↑ Bleeding time Schistocytes (peripheral blood smear) ↑ Serum urea nitrogen and creatinine |
| Management | Supportive care Plasmapheresis, steroids, rituximab Avoid antibiotics as this may precipitate or worsen the condition |
A child with a recent history of bloody diarrhea and a triad of anemia, thrombocytopenia, and renal dysfunction most likely has hemolytic uremic syndrome (HUS). HUS is typically seen in children and is most commonly caused by infection with Escherichia coli O157:H7 (enterohemorrhagic E. coli) and the production of shiga-like toxin. It also may be seen following infection with Shigella dysenteriae and the production of shiga toxin. Both shiga toxin and shiga-like toxin enhance cytokine release resulting in the development of HUS. Note that there is also an atypical form of HUS that is caused by complement gene mutations; however, questions about this topic are not often included in the test. Affected patients typically have a recent or ongoing history of bloody diarrhea, and HUS is characterized by a triad of microangiopathic hemolytic anemia, thrombocytopenia, and renal dysfunction. Each of these components can result in additional symptoms and diagnostic findings as follows:
- Microangiopathic hemolytic anemia → jaundice and dark urine; normocytic anemia on a complete blood count and schistocytes on a peripheral blood smear
- Thrombocytopenia → bleeding and bruising; prolonged bleeding time on coagulation studies
- Renal dysfunction → increased serum urea nitrogen and creatinine concentrations
Treatment of HUS largely consists of supportive care; however, some patients may require treatment with plasmapheresis, corticosteroids, and/or rituximab. Antibiotics should be avoided when enterohemorrhagic E. coli and/or Shigella species are suspected given that they can precipitate or worsen HUS. Antibiotics will cause bacterial cell lysis resulting in the release of intracellular shiga-like toxin or shiga toxin.
Incorrect Answer Explanations
Answer A: Campylobacter jejuni infection can cause gastroenteritis and bloody diarrhea. C. jejuni infections generally occur following contact with contaminated animals, and the pathogen is transmitted in a fecal-oral manner. C. jejuni is associated with the development of Guillain-Barré syndrome, not HUS. Patients with Guillain-Barré syndrome most commonly have symmetric ascending muscle weakness.
Answer C: Henoch-Schonlein purpura (HSP) is a small-vessel vasculitis characterized by palpable purpura of the lower extremities as well as arthritis, arthralgias, abdominal pain, and renal insufficiency (often caused by IgA nephropathy). HSP most commonly occurs after a viral upper respiratory infection, but it can be seen with any viral infection. Here, HSP is unlikely given the absence of joint pain and because HSP would not explain the presence of anemia and thrombocytopenia.
Answer D: Infection with Shigella flexneri can cause a hemorrhagic diarrhea by invading the intestinal epithelium and evoking an immune response. While most Shigella species are known to invade the intestines and cause a hemorrhagic diarrhea, only Shigella dysenteriae is thought to produce shiga toxin. Thus, S. flexneri is not associated with HUS. Also note that, within the United States, infection with enterohemorrhagic E. coli is more common than infection with Shigella species.
Answer E: Enterotoxins produced by Staphylococcus aureus are common causes of secretory diarrhea following ingestion. The toxins most commonly form in contaminated food prior to ingestion. Following ingestion of preformed toxins, enterotoxin activates guanylate cyclase in the intestine. This leads to decreased sodium and chloride resorption and increased fluid retention in the gastrointestinal lumen. This results in watery diarrhea. Symptoms caused by enterotoxin generally appear 1–6 hours after ingestion, only last 24–48 hours, and do not impact organ function outside of the gastrointestinal system. Here, the presence of anemia, thrombocytopenia, and renal dysfunction make S. aureus enterotoxin an unlikely cause of the symptoms in this patient.
Answer F: Streptococcus pyogenes is a common cause of pharyngeal and skin infections, and patients can develop poststreptococcal glomerulonephritis 2–4 weeks after infection. This patient does not have any recent history of an upper respiratory or skin infection, and S. pyogenes would not explain the bloody diarrhea, anemia, and thrombocytopenia.
Answer G: Immune thrombocytopenia often occurs following a viral upper respiratory infection or gastroenteritis. Patients typically have thrombocytopenia, and symptoms can include bruising, bleeding, and epistaxis (nosebleeds). Laboratory studies will show thrombocytopenia and an increased bleeding time. Immune thrombocytopenia is not associated with hemolytic anemia or renal dysfunction and would thus be unlikely in this patient. Additionally, note that viral gastroenteritis most commonly results in watery diarrhea, whereas this patient has bloody diarrhea.
Bottom Line
Hemolytic uremic syndrome is most commonly caused by infection with enterohemorrhagic Escherichia coli (E. coli O157:H7) secondary to the production of shiga-like toxin. Patients typically are children who have a recent/current history of bloody diarrhea and a triad of microangiopathic hemolytic anemia, thrombocytopenia, and renal dysfunction.
TrueLearn Insight
Diagnosis: Immune Thrombocytopenia
| Pathophysiology | Clinical Features | Management |
| Antibodies bind to GpIIb/IIIa on platelets → splenic consumption of platelets Typically seen after a viral illness | Easy bruising and bleeding Epistaxis↓ Platelets↑ Bleeding time | Steroids Intravenous immunoglobulin therapy Splenectomy for refractory idiopathic thrombocytopenic purpura |
Diagnosis: Hemolytic Uremic Syndrome
| Pathophysiology | Clinical Features | Management |
| Commonly seen in children Results from production of shiga-like toxin (from enterohemorrhagic Escherichia coli) or shiga toxin (from Shigella dysenteriae) | Bloody diarrhea Microangiopathic hemolytic anemia Normocytic anemia Schistocytes ↑ Reticulocytes ↑ Total bilirubin Thrombocytopenia and ↑ bleeding time Renal dysfunction → ↑ urea nitrogen and creatinine | Supportive care Plasmapheresis Avoid antibiotics |
Diagnosis: Thrombotic Thrombocytopenic Purpura
| Pathophysiology | Clinical Features | Management |
| More common in adults Inhibition or deficiency of ADAMTS13 (vWF metalloprotease) → ↓ degradation of vWF multimers → platelet adhesion and aggregation | Triad of hemolytic uremic syndrome plus Fever & Altered mental status | Plasmapheresis Steroids Rituximab |
For more information, see:
- Overview of hemolytic uremic syndrome in children: UpToDate
- First Aid for the USMLE Step 1 2019: 132, 419.
- First Aid for the USMLE Step 1 2020: 145.
- First Aid for the USMLE Step 1 2021: 436, 132, 145.
- First Aid for the USMLE Step 1 2022: 434, 130, 143.
- First Aid for the USMLE Step 1 2023: 432, 143, 130.
- First Aid for the USMLE Step 1 2024: 432, 143, 130
Second Sample Question: Hydrochlorothiazide Mechanism Of Action
A 57-year-old African American man comes to the office for follow-up regarding elevated blood pressures. Two months prior, the patient was diagnosed with hypertension due to an elevated blood pressure at multiple office visits. Since then, he has attempted to manage his blood pressure with dietary changes and exercise. Despite a 2.3-kg (5-lb) weight loss during this time, his blood pressure is 150/90 mm Hg on arrival and 152/88 mm Hg on repeat 10 minutes later. He has been tracking his blood pressure at home and notes that his systolic blood pressure ranges between 140 and 160 mm Hg. Given his persistent hypertension, pharmacologic intervention is initiated. Six weeks later, the patient returns to the clinic for follow-up evaluation. He notes that his blood pressures have improved, and his systolic blood pressure now ranges between 125 and 135 mm Hg. Serum laboratory studies are ordered and show the following:
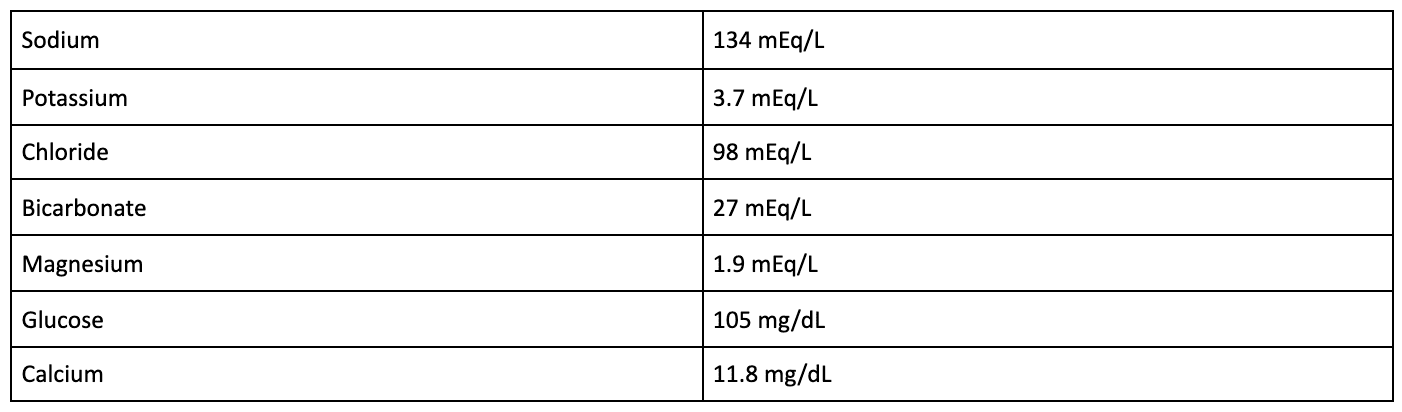
Which of the following best describes the mechanism of action of the pharmacologic agent most likely responsible for this patient’s laboratory findings?
- Blockage of voltage-dependent calcium channels in vascular smooth muscle
- Decreased production of angiotensin II
- Decreased renin secretion
- Increased cGMP-mediated arterial dilation
- Inhibition of sodium chloride reabsorption in the distal convoluted tubule
Explanation
The correct answer is: E
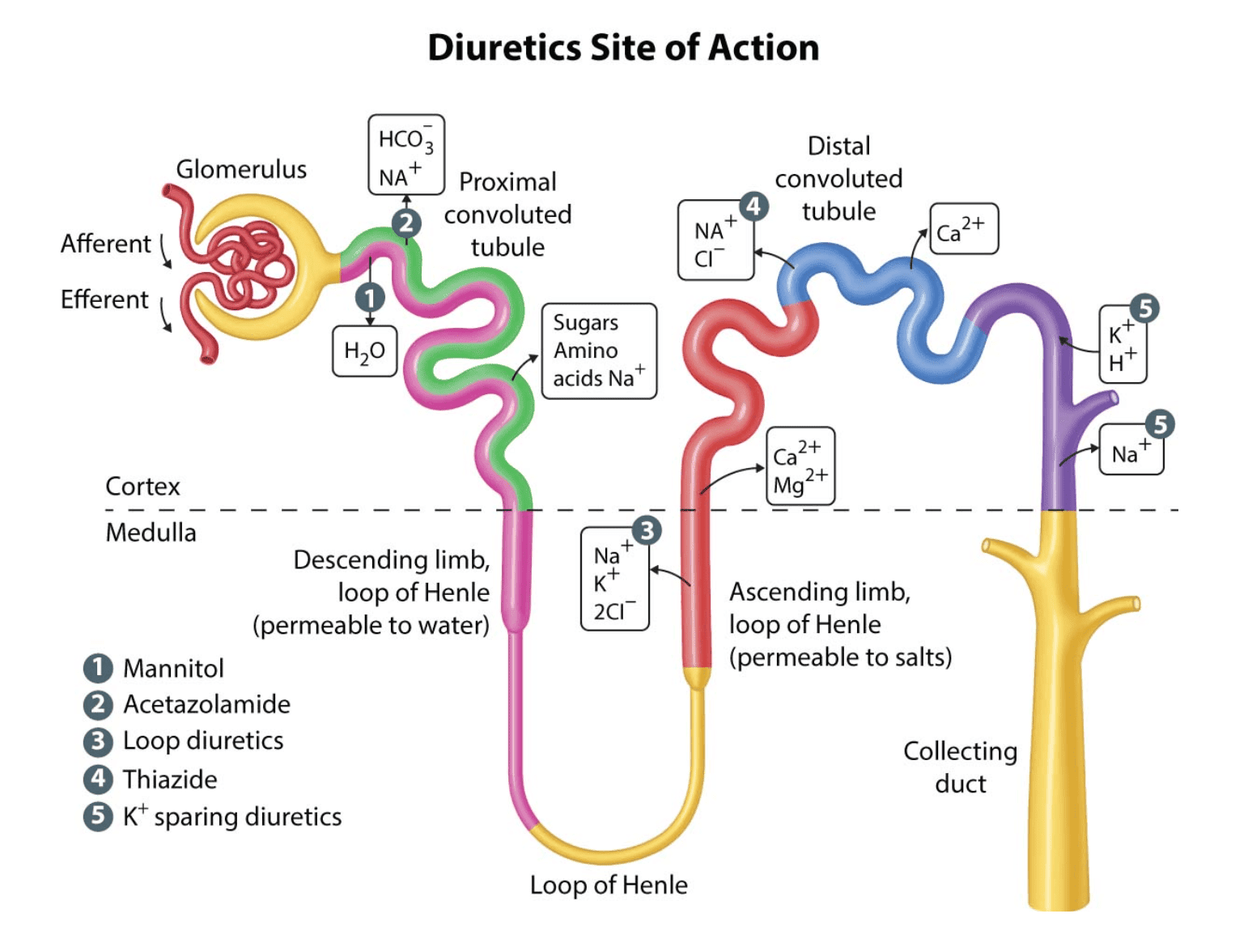
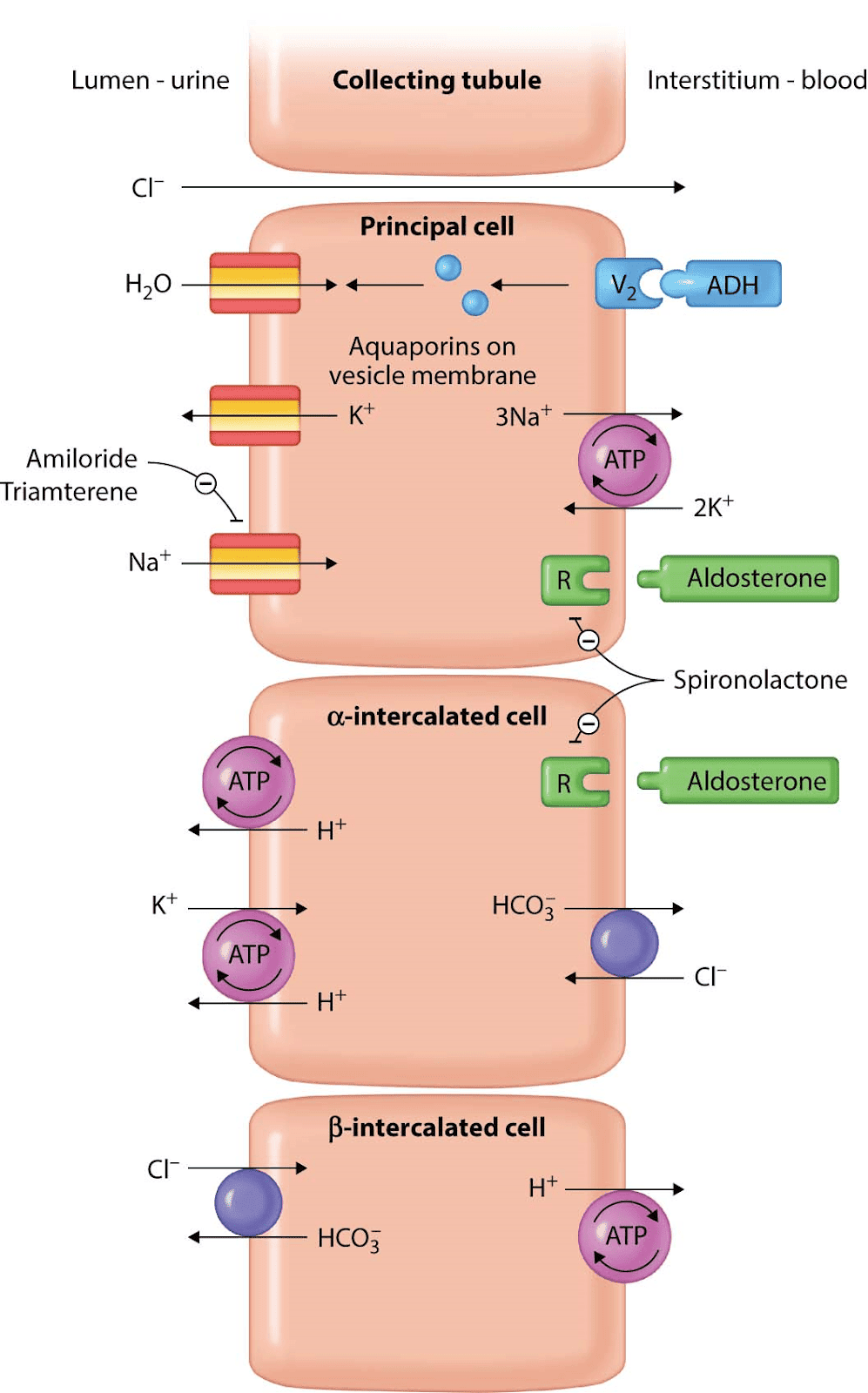
Thiazide diuretics such as hydrochlorothiazide are frequently used in the outpatient treatment of hypertension, especially in African American patients, as they have been shown to be especially beneficial in this population. Thiazides work by inhibiting sodium chloride reabsorption in the early part of the distal convoluted tubule (DCT) that serves to diminish the diluting capacity of the nephron and induces diuresis.
Thiazide diuretics have many adverse events, many of which involve electrolyte imbalances and metabolic disturbances. By inhibiting sodium reabsorption in the DCT, use of thiazide diuretics can result in hyponatremia, as was seen in this patient. In addition, calcium is reabsorbed within the DCT, and thiazide diuretics are known to enhance calcium reabsorption at these transporters. As such, thiazide diuretics will cause a decrease in calcium excretion and can cause hypercalcemia (as was also seen with this patient’s laboratory studies). For this reason, thiazide diuretics can also be used to treat patients with recurrent nephrolithiasis due to calcium-containing stones. However, they should not be used in patients with preexisting hypercalcemia.
Additional adverse events of thiazide diuretics include:
- Hyperglycemia
- Hypokalemia
- Hyperuricemia
- Metabolic alkalosis
- Hyperlipidemia
- Orthostasis
As such, it is important to schedule a patient for follow-up laboratory studies after initiating treatment with a thiazide diuretic. Also note that, in both clinical practice and on the USMLE, patients may have none, one, or multiple of these aforementioned adverse events.
Answer A: Dihydropyridine calcium channel blockers, such as amlodipine, are often used in the treatment of hypertension as they cause vascular smooth muscle relaxation via blockage of voltage-dependent L-type calcium channels. Although they are calcium channel blockers, they are not associated with the development of hypercalcemia or hypocalcemia. Adverse events of these drugs include peripheral edema, weight gain, flushing, dizziness, and gingival hyperplasia.
Answer B: Angiotensin-converting enzyme (ACE) inhibitors, such as lisinopril, are frequently used in the outpatient treatment of hypertension. They are often used in patients with diabetes as these drugs are also nephroprotective in this population. Adverse events of ACE inhibitors include a dry cough, angioedema, and hyperkalemia. They are not associated with hypercalcemia.
Answer C: Beta-blockers are often used in the treatment of hypertension as they decrease both cardiac output and renin secretion. Beta-blockers decrease renin secretion via beta-1 receptor blockade of the juxtaglomerular apparatus cells. Beta-blockers do not cause hypercalcemia. Adverse events of beta-blockers include bradycardia, heart block, sedation, fatigue, exercise intolerance, erectile dysfunction, dyslipidemia (metoprolol only), and asthma or chronic obstructive pulmonary disease exacerbations (nonselective beta-blockers only).
Answer D: Hydralazine is an arterial dilator that may be used in the outpatient treatment of hypertension. Hydralazine causes vasodilation via increased cGMP, which results in smooth muscle relaxation. Given that its main effect is arterial dilation, use of hydralazine can result in rebound tachycardia. Additional adverse events include drug-induced lupus, fluid retention, headache, and angina. Hydralazine does not cause hypercalcemia.
Bottom Line: Thiazide diuretics are frequently used in the outpatient treatment of hypertension and work by inhibiting sodium chloride reabsorption in the distal convoluted tubule in order to induce diuresis. Thiazides also decrease calcium excretion and, as such, can result in the development of hypercalcemia.
For more information, see:
- Mechanism of action of diuretics: UpToDate
- First Aid for the USMLE Step 1 2019: 593, 595.
- First Aid for the USMLE Step 1 2020: 609.
TrueLearn Insight
Tip #1: If you struggle with multistep questions such as this, you can try working backwards from the answer choices. Here, you could have converted each answer to the medication whose mechanism of action it was describing. From there, you would ask yourself: (1) Would this be used to treat hypertension, and (2) could it cause hypercalcemia? Make sure to take advantage of this being a multiple-choice test and learn to work backwards on 2-step and 3-step questions.
Tip #2: The USMLE will frequently ask you questions about a medication without telling you what that medication is. Instead, you will need to identify it based on things like: what is it being used for or what laboratory changes and adverse events developed after using it. Make sure to know the medications that you would use for the treatment of common conditions such as hypertension, diabetes, and dyslipidemia.
Third Sample Question: Primary Sclerosing Cholangitis Risk Factors
A 40-year-old man presents for magnetic resonance cholangiopancreatography (MRCP) as part of ongoing evaluation for fatigue. He notes several other additional symptoms but is unsure if these are related, given that they have been present for many years. Laboratory studies had been ordered by his primary care physician and were remarkable for elevated alkaline phosphatase and direct bilirubin. He occasionally drinks a glass of wine or beer with dinner but denies tobacco or intravenous drug use. MRCP is performed and reveals a series of strictures and dilations in the intrahepatic and extrahepatic biliary ducts. This patient most likely has a history of which of the following additional symptoms?
- Abdominal pain and bloody diarrhea
- Dysarthria and tremor
- Epigastric pain that improves with meals
- Joint pain and hyperpigmentation
- Watery diarrhea
Explanation
The correct answer is: A
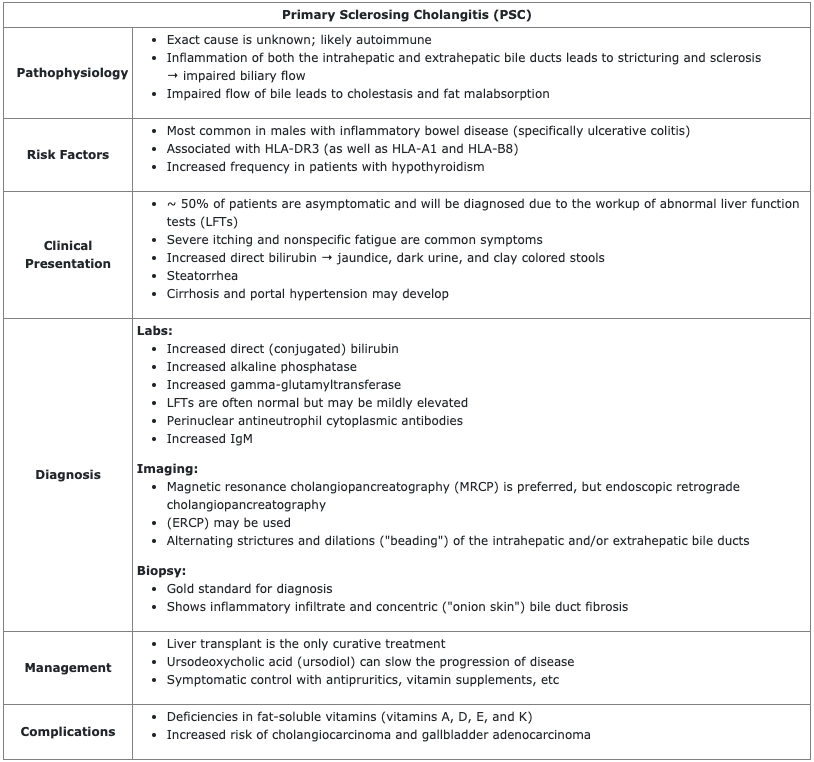
The MRCP findings seen in this patient are indicative of PSC, a form of biliary tract disease that results in concentric bile duct fibrosis of both the intrahepatic and extrahepatic bile ducts. Biliary fibrosis impairs the flow of bile, resulting in an increase in direct (conjugated) bilirubin and alkaline phosphatase on labs. Given that most patients are asymptomatic, PSC is often discovered incidentally due to the evaluation of these abnormal LFTs. When present, common symptoms include fatigue, jaundice, right upper quadrant pain, and steatorrhea.
MRCP or ERCP are useful for making a diagnosis and will demonstrate alternating strictures and dilations (“beading”) of the intrahepatic and/or extrahepatic bile ducts. A biopsy is useful for determining a definitive diagnosis and will show an inflammatory infiltrate as well as concentric bile duct fibrosis.
PSC is most common in male patients with a history of inflammatory bowel disease (most commonly ulcerative colitis); as such, this patient could have noted a prior history of abdominal pain and bloody diarrhea.
Answer B: Wilson disease is caused by an autosomal recessive mutation in the hepatocyte copper-transporting ATPase and results in decreased copper excretion into bile. Subsequent copper accumulation can affect the liver, brain, cornea, and kidneys. In the brain, copper frequently deposits in the basal ganglia and causes symptoms such as dysarthria, dystonia, tremor, and parkinsonism. Wilson disease is not a risk factor for PSC.
Answer C: The presence of epigastric pain that improves with meals is suggestive of a duodenal ulcer. Duodenal ulcers are commonly caused by Helicobacter pylori but may also be found in patients with a gastrinoma (Zollinger-Ellison syndrome). PSC does not increase the risk of duodenal ulcers.
Answer D: Hereditary hemochromatosis is caused by an autosomal recessive mutation that results in increased absorption of iron by enterocytes and symptoms secondary to iron deposition. Patients are frequently approximately 50 years of age and may complain of joint pain, new-onset type 2 diabetes mellitus, hyperpigmentation (“bronze diabetes”), loss of libido, hepatomegaly, jaundice, and cardiomyopathy. Hereditary hemochromatosis is not a risk factor for PSC.
Answer E: In patients with PSC, biliary fibrosis impairs bile flow and can result in fat malabsorption and the presence of steatorrhea. As a result of impaired fat absorption, patients are at risk of developing deficiencies in the fat-soluble vitamins (vitamins A, D, E, and K) and may present with associated symptoms. Watery diarrhea is not seen in patients with PSC.
Bottom Line: Primary sclerosing cholangitis (PSC) most commonly occurs in males with a history of ulcerative colitis. Diagnostic features of PSC include increased alkaline phosphatase and direct (conjugated) bilirubin on labs and imaging that shows dilation and strictures within the intrahepatic and/or extrahepatic bile ducts.
For more information, see:
- Primary sclerosing cholangitis in adults: Clinical manifestations and diagnosis: UpToDate
- First Aid for the USMLE Step 1 2019: 389.
- First Aid for the USMLE Step 1 2020: 395.
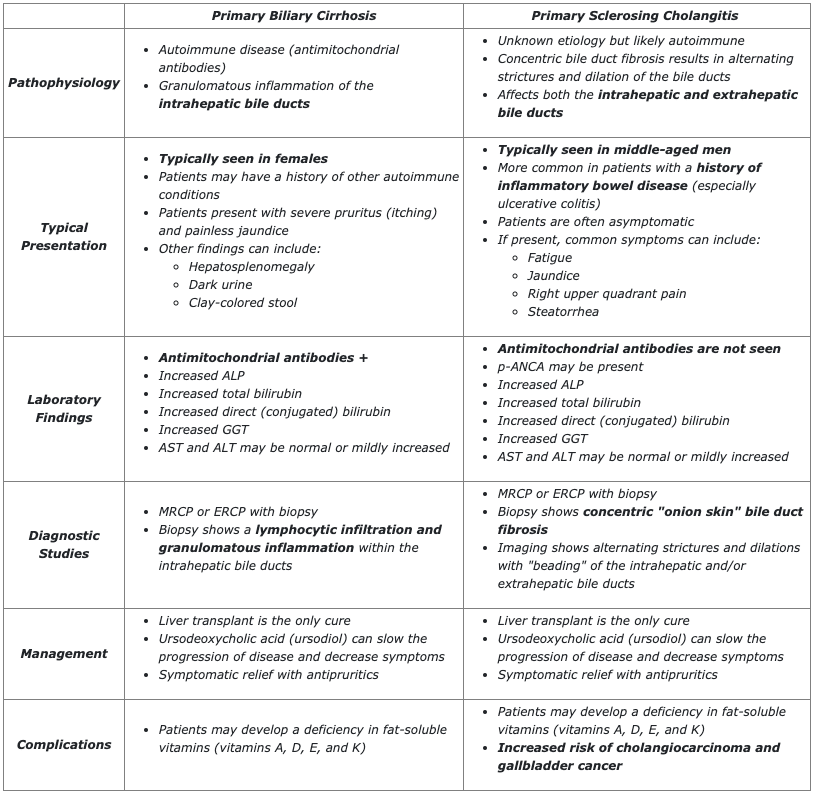
TrueLearn Insight
Make sure to understand the key differences between primary biliary cirrhosis and primary sclerosing cholangitis. Students frequently struggle to differentiate between these two pathologies on the USMLE exams.