Free Internal Medicine Sample Questions
See why TrueLearn is a trusted resource for thousands of medical students and residents. At TrueLearn, we understand that it’s all about the content. That’s why we have high-yield internal medicine practice questions written and screened by high-performing physician authors that are updated on a regular basis to ensure our SmartBanks stay up-to-date with exam blueprint changes. See what we mean with the below internal medicine sample question.
Your First Free Internal Medicine Sample Question (From the 2025-26 Edition)
A 21-year-old male presents to the emergency department with a 5-day history of severe sore throat not relieved by saline mouth rinses and acetaminophen. This morning, he developed high fevers up to temperature 38.5 °C (104.1 °F), shaking chills, dysphagia, left neck pain, and shortness of breath. Past medical history is otherwise unremarkable and he takes acetaminophen as needed. The patient denies using alcohol, illicit substances, or tobacco products.
Vital signs are temperature 39.6 °C (103.3 °F), blood pressure 96/52 mm Hg, heart rate 119/min, respirations 28/min, and oxygen saturation 95% on room air. Physical exam reveals a well-developed male in mild distress. The oropharynx is erythematous with ulcerations located in the left posterior space. Uvula is midline without tonsillar swelling or exudates. The left internal jugular vein (IJV) has a fluctuant cord that is tender to palpation.
There are infiltrates in the apices on chest x-ray. Blood cultures and wound cultures from the mass over left IJV grow anaerobic Gram-negative rods.
Which of the following is the most likely diagnosis?
- A. Bacterial pharyngitis
- B. Infectious endocarditis
- C. Jugular vein suppurative thrombophlebitis
- D. Peritonsillar abscess
- E. Retropharyngeal abscess
Answer and Explanation
The correct answer is: C
Suppurative thrombophlebitis refers to venous thrombosis associated with inflammation in the setting of bacteremia. Infection involving the jugular vein is called Lemierre syndrome, also known as postanginal sepsis or necrobacillosis. The carotid sheath is located in the posterior lateral pharyngeal space and contains the internal carotid artery, internal jugular vein, and vagus nerve (cranial nerve X). Patients develop Lemierre syndrome from antecedent infection within the oropharynx–pharyngitis, infectious mononucleosis, primary dental infection–that spreads to the parapharyngeal or lateral pharyngeal space.
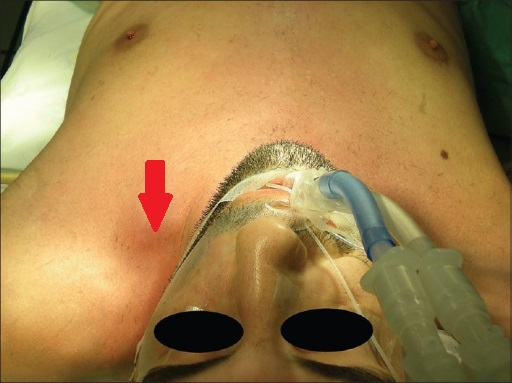
The most common organism associated is Fusobacterium necrophorum, a gram-negative anaerobic rod found in oral flora. Other organisms include Fusobacterium spp., Eikenella corrodens, Streptococci spp., Bacteroides spp., and Porphyromonas asaccharolytica. Lemierre syndrome may occur from hematogenous spread via indwelling vascular catheters; the common organisms associated are skin flora and nosocomial pathogens. Patients are healthy young adults who develop high fevers and rigors with respiratory distress following pharyngitis.
Examination may reveal an erythematous or ulcerated oropharynx and edema or tenderness overlying the jugular vein or intravascular catheter.
Chest x-ray will demonstrate infiltrates from septic emboli that can progress into abscesses or empyema. Suspect Lemierre syndrome in additional patients with persistent bacteremia for more than 72 hours despite antibiotics, especially in the presence of indwelling catheters. Make the diagnosis with cultures of blood or wound and imaging (CT scan of neck with contrast reveals filling defects or thrombus in the internal jugular vein).
Treatment is multifaceted. First, remove the indwelling catheter or the oral infection nidus. Second, cover empirically for the most common organisms with beta-lactamase resistant beta-lactam (ex. ampicillin-sulbactam, piperacillin-tazobactam, ticarcillin-clavulanate) or carbapenem if beta-lactam allergic. Add vancomycin if the infection is catheter-associated. Duration is a minimum of two weeks intravenous followed by oral therapy for four weeks total or until resolution of pulmonary abscesses or clinical improvement. Surgery may be beneficial for ongoing sepsis or no response to antibiotics. Methods include drainage, ligation, or excision of internal jugular vein with incision and drainage of adjacent infection. Anticoagulation is rarely recommended unless the thrombus extends.
Incorrect Answer Explanations
Answer A: The most common cause of bacterial pharyngitis is Streptococcus pyogenes group A, a gram-positive coccus that grows in chains. It does not present with septic emboli in the lungs.
Answer B: Infectious endocarditis is characterized by new-onset murmur with presence of valvular vegetations and positive blood cultures for likely pathogens or minor symptoms including embolic disease, immune complex deposition, high fevers, certain risk factors, or organisms isolated in cultures. This patient has high fevers and septic emboli; however, he does not have a murmur, and his presentation can be explained by a different infectious process.
Answer D: Peritonsillar abscesses are infections that involve the tonsils from antecedent pharyngitis. Physical exam reveals ipsilateral tonsillar swelling and contralateral uvula deviation. CT neck will demonstrate fluid collection over the involved tonsil. This patient has a presentation consistent with suppurative thrombophlebitis.
Answer E: Retropharyngeal abscess presents initially as sore throat, then progresses into neck pain with dysphagia and dysphonia. Patients have a “muffled potato” voice with widened retropharyngeal space. The most common organism is Streptococcus spp. This patient had pharyngitis that progressed into left IJV suppurative thrombophlebitis.
Bottom Line
Lemierre syndrome is the suppurative thrombus infection involving the internal jugular vein. Findings include high fevers, pharyngitis, septic emboli, and persistent bacteremia in the setting of oral infections or intravascular catheters.
Your Second Free Internal Medicine Sample Question
A 35-year-old man presents to the clinic with elevated blood pressure. His blood pressure had been previously normal but climbed up to 150-160/90-100 mm Hg in the past 2 months. He has been feeling irritated by his blood pressure troubles, compounded by his recent decision to quit smoking 3 months ago. He denies headaches, diarrhea, or leg cramping. He has been chewing gum constantly to satisfy his oral cravings for cigarettes and found a licorice-flavored brand that he enjoys best. He is feeling well otherwise. He takes no medications and drinks 1 to 2 beers a week.
Blood pressure on exam is 154/96 mm Hg in the right arm and 150/92 mm Hg in the left arm. Physical exam is remarkable for a well-developed male of normal body habitus in no acute distress. No papilledema is observed, and no abdominal or renal bruits are appreciated. He chews gum throughout the entire visit.
Laboratory studies are shown.
| Parameter | Patient Value | Reference Range |
| Sodium (mEq/L) | 147 | 135 – 145 |
| Potassium (mEq/L) | 3.0 | 3.5 – 5.5 |
| Serum bicarbonate (mEq/L) | 30 | 23 – 30 |
| Plasma aldosterone (ng/dL) | 0.5 | ≤10 |
| Plasma renin, supine (ng/mL/hr) | Undetectable | 0.3-2.5 |
Which of the following is the most appropriate next step in management?
- A. Ask the patient to abstain from the licorice-flavored gum
- B. Check his adrenocorticotropic hormone level
- C. Perform an oral salt load
- D. Perform genetic testing for 11-beta-hydroxylsteroid dehydrogenase type 2 gene mutations
- E. Send the patient for a computed tomography scan of the abdomen and pelvis
Answer and Explanation
The correct answer is: A
Hyperaldosteronism is suspected in patients with hypertension accompanied by hypernatremia, hypokalemia, and metabolic alkalosis. The diagnosis lies in the amount of aldosterone and renin present. In primary hyperaldosteronism, aldosterone is elevated and the plasma aldosterone concentration (PAC) to plasma renin concentration (PRC) ratio is greater than 20 to 30. In secondary hyperaldosteronism, aldosterone is elevated, but the PAC:PRC ratio is < 20 because the renin is elevated in relation. There are syndromes that mimic hyperaldosteronism but are characterized by low aldosterone levels because there is a nonmineralocorticoid excess. Chronic licorice ingestion fits into this category.

In order to understand how licorice can cause a syndrome similar to hyperaldosteronism, it is necessary to review the enzymes involved in this process. In normal adrenal physiology, there is an excess of cortisol in comparison to aldosterone (100:1), but both hormones bind renal mineralocorticoid receptors with equal affinity. To avoid excess mineralocorticoid effects, the enzyme 11-beta-hydroxylsteroid dehydrogenase type 2 (11-B-HSD2) inactivates cortisol via conversion to cortisone. This enzyme, however, is competitively inhibited, and its gene expression is decreased in the setting of chronic black licorice ingestion. Black licorice is derived from the root of Glycyrrhiza glabra and contains glycyrrhetinic acid, the compound responsible for inactivating 11-B-HSD2. Licorice-like products (eg, flavored chewing gum or chewing tobacco) contain carbenoxolone, another compound capable of inhibiting 11-B-HSD2. This leads to normal cortisol levels with net increase in mineralocorticoid activity. Chronic ingestion of licorice in small amounts (50 g/d) can cause elevated blood pressure within 2 weeks.
The treatment involves cessation of licorice (or licorice-like product) intake. Some patients may need potassium-sparing diuretics or potassium supplements for the first week while the effects of licorice wear off. Abnormal function of 11-B-HSD2 is also present in apparent mineralocorticoid excess (AME), an autosomal recessive condition associated with failure to thrive and severe hypertension in children, in addition to pseudo-hyperaldosteronism; the ratio of urinary cortisol to urinary cortisone is used to confirm the diagnosis, and it will be greater than 5 to 18 (normal is 0.3-0.5). In chronic licorice consumption, however, the ratio will be slightly elevated (around 1) to differentiate it from AME.
Incorrect Answer Explanations
Answer B: Ectopic adrenocorticotropic hormone (ACTH) can cause pseudo-hyperaldosteronism secondary to non-mineralocorticoid excess by increasing cortisol levels. However, this patient does not have features associated with Cushing syndrome that would indicate the need to quantify ACTH.
Answer C: In a patient with primary hyperaldosteronism, the confirmation test is an oral salt load. However, this patient has low aldosterone because of his pseudo-hyperaldosteronism secondary to non-mineralocorticoid excess.
Answer D: Apparent mineralocorticoid excess (AME) is a genetic disorder associated with the absence of 11-beta-hydroxylsteroid dehydrogenase type 2 (11-B-HSD2), leading to clinical symptoms and lab values associated with pseudo-hyperaldosteronism from non-mineralocorticoid excess. However, this disorder usually presents early in life with failure to thrive and severe hypertension. In addition, this patient’s licorice consumption should be curtailed prior to further workup for this syndrome.
Answer E: Once you confirm primary hyperaldosteronism, you send the patient for a CT of the abdomen and pelvis to look for adrenal adenoma or carcinoma. This clinical scenario is indicative of non-mineralocorticoid excess, not primary hyperaldosteronism.
Bottom Line
Ingestion of black licorice or licorice-containing products can cause pseudo-hyperaldosteronism characterized by hypertension, hypernatremia, hypokalemia, and metabolic alkalosis with low aldosterone and renin levels due to non-mineralocorticoid excess involving decreased inactivation of cortisol to cortisone through competitive inhibition of 11-B-HSD2 by glycyrrhetinic acid.
For more information, see:
- “Apparent mineralocorticoid excess syndromes (including chronic licorice ingestion).” On UpToDate.
- Seifter JF. “Potassium disorders.” Goldman-Cecil Medicine. 26th ed. Philadelphia: Saunders, 2020. 724-731. Print.
- Image obtained from Wikimedia Commons. Used with permission.
Get More Free Internal Medicine Questions
Ready for more practice questions? Sign up for a free trial of TrueLearn’s SmartBank.