Free OBGYN Board Review Sample Questions
TrueLearn is a trusted resource for so many OB/GYN residents. We understand that it’s all about the content. That’s why we have high-yield ABOG and CREOG practice questions written and screened by high-performing physician authors that are updated on a regular basis to ensure our SmartBanks stay up-to-date with exam blueprint changes. See what we mean with the below free OB/GYN board review questions.
Your Free OBGYN Practice Question for CREOG
On postoperative day 2 following a total abdominal hysterectomy, a patient complains of numbness of her thigh and difficulty getting out of bed. On examination she has weakness with hip flexion and knee extension and she has a decrease in sensation over her anterior thigh. Which nerve was injured at the time of her surgery?
- A. Femoral nerve
- B. Genitofemoral nerve
- C. Ilioinguinal nerve
- D. Obturator nerve
- E. Sciatic nerve
The Answer and Explanation
Weakness with hip flexion and knee extension and numbness of the anterior aspect of the thigh can be seen with iatrogenic femoral nerve injury.
Did you get it right? The correct answer is A.
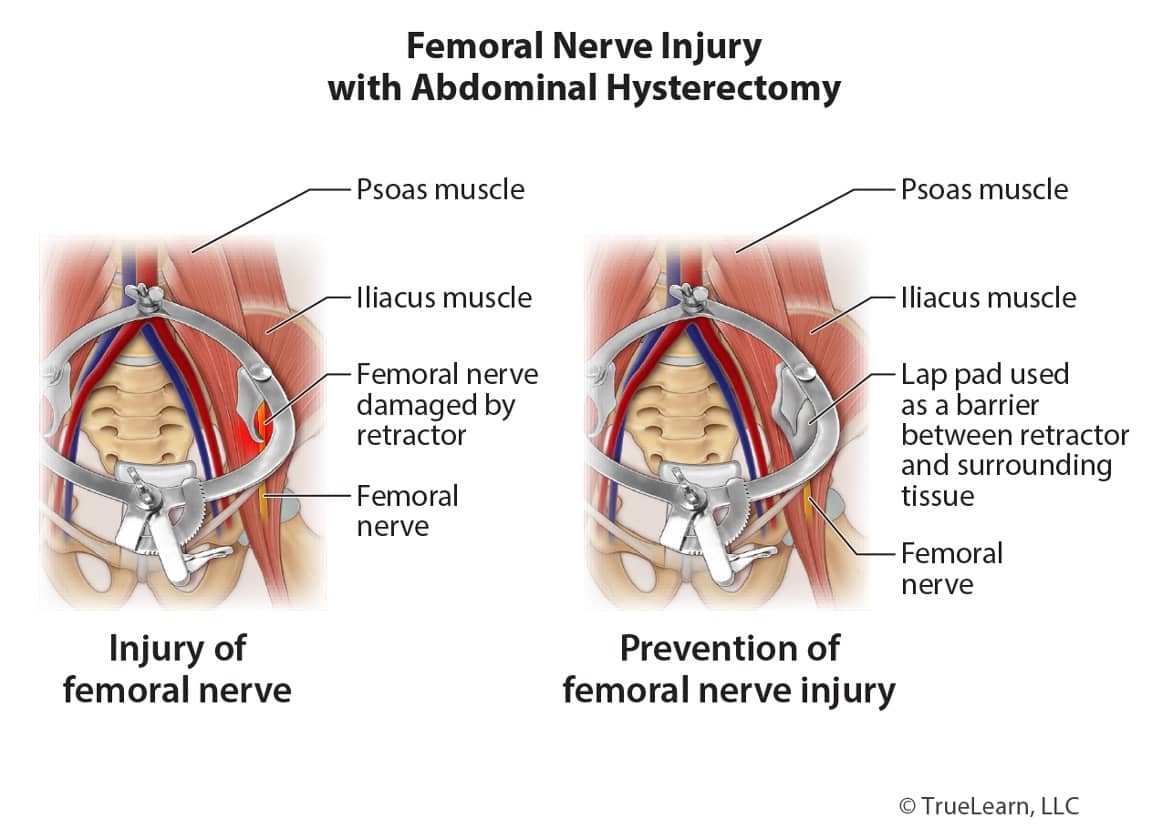
Gynecologic surgery is the most common cause of iatrogenic femoral nerve injury and it can occur in up to 10% of abdominal hysterectomies. Compression is the most common cause and it leads to an ischemic neuropathy. The compression is usually due to the placement of retractor blades. The femoral nerve is most often injured where it runs along the psoas muscle or as it passes beneath the inguinal ligament. Following injury, motor function will present as weakness or an inability to flex at the hip or to extend at the knee and the patellar reflex will also be absent or impaired. Impairment in sensory function will present as a paresthesia over the anterior and medial thigh (innervated by the anterior cutaneous branches of the femoral nerve) and medial aspect of the calf.
During surgery, care should be taken to ensure that retractor blades retract only the rectus abdominis and not the psoas muscle and folded laparotomy towels can be used as cushioning between the retractor and skin in order to reduce the risk of femoral nerve injury. The femoral nerve can also be injured where it passes beneath the inguinal ligament due to prolonged compression in lithotomy position; efforts should be made to minimize sharp flexion, abduction, and external hip rotation.
| General Risk Factors For Post-Operative Neuropathy |
| Prolonged surgery duration Thin patients Patients who smoke or have alcohol dependency Patients with diabetesUse of self-retaining retractors |
Nerve Injuries and Gynecologic Surgery
| Effects of Nerve Injury | Mechanism of Nerve Injury in Gynecologic Surgery | Risk Factors |
| Femoral Nerve | ||
| Numbness of anterior and medial thigh Weakness of quadriceps and iliopsoas muscles | Compression against the pelvic sidewall Compression at inguinal ligament due to hyperflexion of the thigh during vaginal surgery | Wide Pfannenstiel incision Narrow pelvis Use of self-retaining retractors |
| Obturator Nerve | ||
| Numbness of inner thigh Weakened adduction | Injury during pelvic lymph node dissection Injury during placement of transobturator tape | Paravaginal defect repair Excision of endometriosis, lymph node excision, or dissection along the pelvic sidewall |
| Common Peroneal Nerve (Common Fibular Nerve) | ||
| Difficulty with dorsiflexion of foot Numbness or paresthesia of dorsal aspect of foot and lateral shin | Compression at lateral aspect of fibula in stirrups | Prolonged surgery, inadequate padding of pressure points |
| Genitofemoral Nerve | ||
| Numbness or paresthesia of labia and upper medial thigh No motor weakness | Compression from retractor blades Injury during dissection around external iliac lymph nodes or iliac vessels | Removal of pelvic mass adherent to pelvic sidewall |
| Pudendal Nerve | ||
| Labial and perineal pain No sensory loss | Entrapment or injury during placement of suture in arcus tendineus fasciae pelvis | Sacrospinous ligament fixation Pelvic floor reconstruction procedures |
| Brachial Plexus | ||
| Motor and sensory deficits of upper extremity | Compression, stretching, or pressure-induced ischemia | Steep Trendelenberg and longer operating times with robotic surgery Use of shoulder plates or blocks Use of arm boards Lateral flexion of the neck |
| Sciatic Nerve | ||
| Sensory and motor deficits of lower extremity | Stretch injury from hip flexion or external hip rotation | Lithotomy position with excessive external hip rotation |
| Ilioinguinal Nerve and Iliohypogastric Nerve | ||
| Burning sensation in the suprapubic area, labia, or proximal thighs | Transection from transverse abdominal incisions or entrapment in suture | Wide transverse abdominal incision |
Incorrect Answer Explanations
Answer B: An injury to the genitofemoral nerve can cause numbness or paresthesia of the upper medial thigh and does not cause motor deficit.
Answer C: The iliohypogastric and ilioinguinal nerves are most commonly injured when a low transverse incision is made. Patients usually complain of sharp, burning pain from the incision site that radiates to the suprapubic area, labia, or thighs. Significant loss of sensation is unusual as the suprapubic area receives sensory innervation from several different supplies. The iliohypogastric and ilioinguinal nerves can be injured due to surgical trauma or entrapment in suture or scar tissue. Risk of injury can be minimized by keeping the fascial incision within the lateral borders of the rectus muscles.
Answer D: An obturator nerve injury can cause weakened thigh adduction and decreased sensation to the medial thigh.
Answer E: A sciatic nerve injury can also cause sensory and motor deficits affecting the lower extremity, but the specific deficits are different from those caused by a femoral nerve injury. The sciatic nerve is at risk to stretch injury during surgeries performed with the patient in lithotomy position.
The sciatic nerve is responsible for innervation to the muscle groups that perform hip extension and knee flexion. The sciatic nerve divides into the tibial nerve and the common peroneal nerve in the popliteal fossa. The common peroneal nerve innervates muscles responsible for knee flexion and foot dorsiflexion and eversion. The tibial nerve innervates muscles responsible for thigh extension, knee flexion, and foot plantarflexion and inversion.
A sciatic nerve injury can result in decreased sensation to the lower leg and foot, with normal sensation along the medial calf and arch of the foot which are instead supplied by the saphenous nerve (a branch of the femoral nerve). Sciatic nerve injury does not cause sensory loss of the thigh.
Bottom Line
The femoral nerve can be injured during gynecologic surgery, most often due to compression from retractor blades as it runs along the psoas muscle (in abdominal cases) or where it passes beneath the inguinal ligament (in lithotomy position). Injury can cause weakness with hip flexion and knee extension and numbness of the anterior aspect of the thigh.
For more information, see:
- William Gynecology, 4th ed. Chapter 40: Intraoperative Considerations.
- Nerve injury associated with pelvic surgery. UpToDate.
The Next Free OBGYN Practice Question for ABOG
A 22-year-old woman presents for worsening hirsutism over the past 6 months as well as temporal balding. On exam, the physician notes a Ferriman–Gallwey score of 18. Lab tests return and are significant for total testosterone of 62 ng/dL, a normal 17-hydroxyprogesterone level, and a DHEA-S level of 850 mcg/dL. What is the next BEST step in the workup of her hirsutism?
- A. ACTH stimulation test
- B. Adrenal CT
- C. Observation
- D. MRI of the pelvis
- E. Renal US
Answer and Explanation
Hirsutism is defined as excessive male-pattern hair and facial and body hair that affects 5%–10% of reproductive-age women.
Did you get it right? The correct answer is B.
The major circulating hormones in women (in descending order) are:
- DHEA-S
- DHEA
- androstenedione
- testosterone
- dihydrotestosterone (DHT)
Evaluation of hirsutism includes measurement of total testosterone, DHEA-S, and 17-hydroxyprogesterone. DHEA-S is derived almost exclusively from the adrenal glands, and the upper limit of normal is typically 350 mcg/dL but can vary between laboratories. DHEA-S levels greater than 700 mcg/dL may indicate a rare androgen-secreting adrenal tumor such as an adrenal adenoma or carcinoma.
An adrenal CT is the imaging study of choice due to excellent sensitivity and specificity in detecting these tumors.
Incorrect Answer Explanations
Answer A: Adrenocorticotropic hormone stimulation test would be an appropriate next step in the workup of a patient with an elevated 17-hydroxyprogesterone level and concern for nonclassic congenital adrenal hyperplasia (NCCAH). This test should be performed when the 17-hydroxyprogesterone level is between 200 and 800 ng/dL. An ACTH stimulation test is thus performed, and the 17-hydroxyprogesterone level is rechecked. If it is over 1500 ng/dL, NCCAH is diagnosed.
Answer C: Observation is not an appropriate next step because her DHEA-S level is elevated above normal, which may signify a possible androgen-secreting adrenal tumor.
Answer D: Evaluating for an adrenal adenoma is best accomplished by an adrenal CT. A pelvic MRI may be useful if evaluating for pelvic pathology, including malignancy or concern for ovarian masses if transvaginal ultrasonography is inconclusive; however, it is not the next best step when assessing adrenal pathology.
Answer E: The gold-standard imaging modality for adrenal masses is an adrenal CT. Ultrasonography has unacceptably low sensitivity and specificity in this scenario.
Bottom Line
DHEA-S levels greater than 700 mcg/dL may indicate a rare androgen-secreting adrenal tumor, such as an adrenal adenoma or carcinoma. An adrenal CT is the gold-standard imaging modality in detecting an adrenal tumor.
For more information, see:
- Speroff’s Clinical Gynecologic Endocrinology and Infertility, 9th ed. Chapter 12: Hirsutism.
- Williams Gynecology, 4th ed. Chapter 18: Polycystic Ovarian Syndrome and Hyperandrogenism.
- Hirsutism. StatPearls.