Free NBME Shelf Exam Sample Questions
See why TrueLearn is a trusted resource for thousands of medical students and residents. At TrueLearn, we understand that it’s all about the content. That’s why we have high-yield NBME practice questions written and screened by high-performing physician authors that are updated on a regular basis to ensure our SmartBanks stay up-to-date with exam blueprint changes. Below is a free NBME sample question so you can see first-hand what we mean.
Your First Free NBME Sample Question
A 55-year-old man presents to the emergency department with chest pain and fever. The chest pain started 12 hours prior to arrival and is exacerbated by deep inspiration. He states that he has recently had a heart attack approximately one month prior and is concerned he may be having another one. His temperature is 38.3°C (101°F), pulse is 80/min, respirations are 16/min, and blood pressure is 160/90 mm Hg. Pulse oximetry shows an oxygen saturation of 99% on room air. Physical examination shows an anxious appearing man. An ECG is obtained and reveals diffuse ST elevations and PR depressions and chest imaging is pending.
Which of the following is the most likely diagnosis?
- A. Acute MI
- B. Left ventricular aneurysm
- C. Pneumonia
- D. Post cardiac injury syndrome
- E. Pulmonary embolism
Answer and Explanation
The correct answer is: D
The patient in the above scenario has post-cardiac injury syndrome, also known as Dressler syndrome. Dressler syndrome is an autoimmune process that occurs 2-10 weeks after an MI. Dressler syndrome often presents with fever, pericarditis, pleural effusions, leukocytosis, and an elevated erythrocyte sedimentation rate. Pericarditis is inflammation of the pericardial sac surrounding the heart. Pericarditis is characterized by chest pain that is constant and pleuritic in nature. It can be exacerbated by lying flat. Classic ECG findings in pericarditis include diffuse ST elevations and PR depressions. Initial treatment includes non-steroidal anti-inflammatory drugs and colchicine. In refractory disease, steroids may be indicated. For this patient who is post MI, aspirin would be the preferred drug rather than ibuprofen or other non-steroidal anti-inflammatory drugs.
The image below is an ECG of a patient with pericarditis changes.
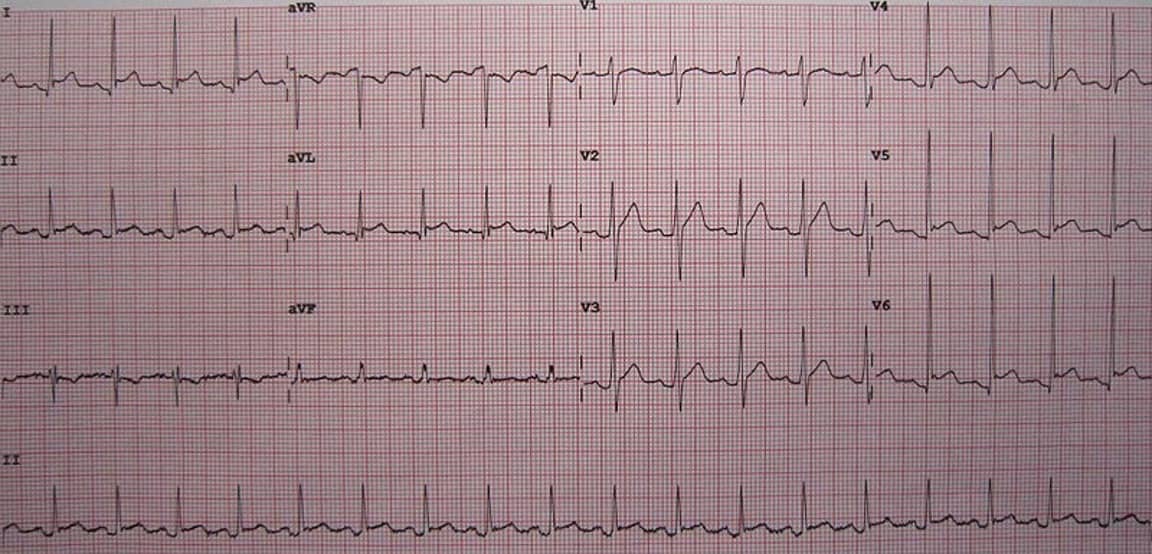
(Open Access Image/James Heilman, MD.)
Incorrect Answer Explanations
Answer A: An acute MI often presents with substernal chest pain or pressure radiating to the left jaw or arm that is associated with shortness of breath, diaphoresis, nausea, and light-headedness. In an ST-elevation MI, there will be ST elevations present in 2 or more contiguous leads with reciprocal changes. In this case, the patient presents with positional chest pain that is pleuritic in nature as well as an ECG demonstrating diffuse ST elevation. These findings are not likely to be a new acute MI.
Answer B: Patients with a ventricular aneurysm invariably have preceding MIs and also present with chest pain. However, this patient had a fever which is uncommon in patients with ventricular aneurysms. Furthermore, these patients also present with signs of heart failure, such as crackles on lung exam or abnormal oxygenation. In this patient, there were no signs or symptoms overly suggestive of heart failure.
Answer C: Pneumonia often presents with fever, productive cough with purulent sputum, dyspnea, and pleuritic chest pain. Pneumonia will be evident as a consolidation on a chest radiograph. In this case, the patient had no cough and also presents with ECG changes which are unlikely to occur in the setting of pneumonia.
Answer E: Pulmonary embolism typically presents with sudden-onset dyspnea, pleuritic chest pain, and hypoxia. In addition, diffuse ST elevations and PR depressions on ECG are not commonly seen in pulmonary embolism. Rather, sinus tachycardia may be appreciated.
Bottom Line
Dressler syndrome is an autoimmune process that occurs 2-10 weeks after a myocardial infarction. Dressler syndrome often presents with fever, pericarditis, pleural effusions, leukocytosis, and an elevated erythrocyte sedimentation rate.
TrueLearn Insight
Be aware of the complications associated with myocardial infarction:
| Time Post MI | Complication |
| <4 hours | arrhythmias, cardiogenic shock, congestive heart failure |
| 4-24 hours | arrhythmias |
| 1-3 days | fibrinous pericarditis |
| 4-7 days | ventricular free wall rupture, interventricular wall rupture, papillary muscle dysfunction |
| weeks to months | Aneurysms, mural thrombus, Dressler syndrome |
For more information, see:
- Acute Pericarditis: Clinical Presentation and Diagnostic Evaluation on UpToDate
- Acute Pericarditis on Medscape
Get More Free NBME Sample Questions
Want to keep checking out what makes TrueLearn’s NBME practice questions so unique? Sign-up for a free trial of our USMLE Step 2 + NBME Shelf question bank. Or if you’re ready, take a look at our subscriptions.