Why You Should Include Spaced Repetition and Practice Retrieval in Your Medical School Curriculum

The rigor of the medical school curriculum is well known and educators know that for students to outperform on the USMLE® Step 1, they must establish a solid knowledge foundation during pre-clinical years. Spaced repetition has proven to be effective in helping medical students master complex concepts and, just as importantly, retain them long-term—thus empowering students to continue performing well in clinical years, leading to ideal outcomes on Step 2 CK and NBME Shelf exams. Embracing spaced repetition also allows students to foster lifelong learning habits, ensuring they are adequately prepared for future practice and competent in delivering high-quality patient care.
Rooted in the science of memory, the spaced repetition method leverages the brain’s natural functions to ensure that material is reviewed just before it’s forgotten. How does this make learning more efficient and effective?
What is the Space Repetition Method
Spaced repetition is a powerful learning strategy that involves exposing learners to similar material at regular intervals. As concepts are retained, the spacing between reviews is gradually increased, which helps embed knowledge more deeply into long-term memory. This technique is based on Hermann Ebbinghaus’ 1885 research on the spacing effect, which found that when repetitions are spaced over time, they produce stronger and more durable memories compared to repetitions that are closely spaced.
One critical application of spaced repetition is its ability to circumvent what Ebbinghaus termed the “forgetting curve,” a phenomenon where memories fade over time regardless of initial learning success. Spaced repetition helps mitigate this effect by reviewing course content at increasing intervals, thereby lessening the curve and committing information to long-term memory. By continually reinforcing knowledge through practice retrieval—the active recall of information—medical students can optimize their study time, reducing the need to re-learn content and instead focusing on mastering more complex concepts and developing higher-order thinking skills.
To understand the effects of spaced repetition the impact it can have on students’ learning and delivery of quality patient care, let’s explore the research on both learning techniques.
What Research Says About Spaced Repetition
In a randomized cluster crossover trial comprising 354 clinicians conducted at the Vanderbilt University Medical Center, researchers sought to determine the effects of spaced repetition and retrieval practice on prescribing patterns.1 Over a four-week period, participants completed an educational module by answering a daily quiz of multiple-choice questions via a mobile phone app. The results showed a statistically significant jump in the likelihood of prescribing behaviors being consistent with evidence-based practices. In this instance, the odds of the clinicians prescribing balanced crystalloids over normal saline doubled.
This research suggests that evidence-based strategies — spaced repetition and retrieval practice — could enhance clinical practice.2 To achieve such improvements, physicians and clinicians must be familiar with such active learning strategies, and Wlodarczyk & Dhaliwal2 of the University of California San Francisco (UCSF) School of Medicine suggest that integrating learning science into medical education would enable schools to produce future practitioners who have good learning hygiene and are poised to embrace learning science to elevate clinical practice, thus delivering optimal healthcare services.
The Research on Teaching Medical Students Using Spaced Repetition
One approach to establishing a strong understanding of learning science among medical students is simple–teach it. Leveraging a near-peer approach, UCSF implemented an interactive session for first-year students to teach them evidence-based learning strategies. Following the session, 89.7% of students reported learning a new strategy from peers, and 88.6% reported being very likely to implement what they learned.3
Another option is for faculty to integrate evidence-based strategies into the curriculum from day one to promote effective teaching and learning while modeling to students techniques that support improved knowledge acquisition, retention, and recall. What’s a by-product of this pedagogy? Medical students master concepts more quickly and retain information longer, helping them perform optimally on USMLE® Step exams.
Integrating a proven solution into the medical school curriculum
Built on a robust data analytics engine, TrueLearn provides programs and faculty with invaluable performance metrics in real-time so they can track progress, uncover weak and strong content areas, spot curricular gaps and redundancies, and identify at-risk students to remediate promptly, increasing their chances of obtaining a first-time pass.
Additionally, TrueLearn’s proprietary tagging feature allows custom tagging and mapping of items directly to the curriculum. This benefits both faculty and students: educators can leverage this to incorporate regular formative assessments to easily track and measure student progress or deploy the questions as student or class assignments. On the other hand, students can utilize the same functionality to self-test with items relevant to their learning needs, study plans, and day-by-day coursework while simultaneously preparing for the boards from day one and throughout the program’s entirety. Integrating the TrueLearn solution into the curriculum thus enables programs and faculty to ensure optimal academic and exam outcomes and help students develop lifelong learning habits that will serve them well beyond the classroom and clinical settings.
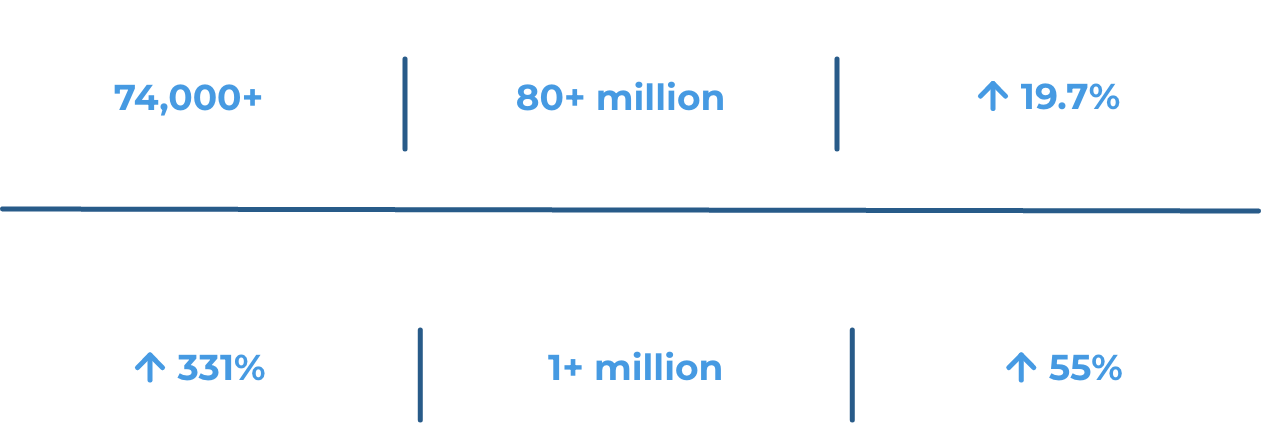
TrueLearn utilizes the principles of cognitive science and leverages evidence-based techniques such as retrieval practice, interleaving, varied practice, and spaced repetition to deliver engaged, active learning and simulated USMLE® test-taking experiences. Integrated with Picmonic audio-visual mnemonic videos — proven to increase long-term retention by 331% — educators can access a full suite of learning and assessment tools to enhance lectures, courses, and clinical experiences, advancing students’ learning, concept mastery, long-term retention, and critical thinking skills.
TrueLearn’s impact on student learning and exam outcomes is research-proven, so medical schools nationwide trust our solution to deliver academic and exam excellence.
How can educators leverage such learning strategies to drive USMLE® success for their program and students? Our Faculty Resource breaks it down.
References & Footnotes
1 McEvoy MD, Dear ML, Buie R, et al. Effect of smartphone App–Based education on clinician prescribing habits in a learning health care system. JAMA Network Open. 2022;5(7):e2223099. doi:10.1001/jamanetworkopen.2022.23099
2 Wlodarczyk S, Dhaliwal G. The learning sciences meet the learning health system. JAMA Network Open. 2022;5(7):e2223113. doi:10.1001/jamanetworkopen.2022.23113
3 Ransohoff A, Boscardin C, Hauer KE, Wlodarczyk S. Rethinking how to introduce the learning sciences: a near-peer approach. Med Sci Educ. 2020;31(1):45-47. doi:10.1007/s40670-020-01142-5
*The USMLE® and National Board of Medical Examiners® (NBME®) subject exams are trademarks of the National Board of Medical Examiners. This content is not endorsed or approved by NBME.